NHS 70 series - How has the role of women in the NHS changed since its inception?
London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png Wednesday 20 June 2018Nearly seventy years after its creation, women are beginning to occupy more and more leadership roles in the NHS, however this has not always been the case.
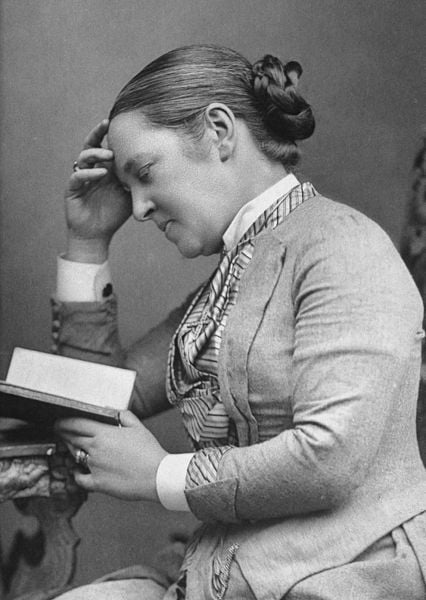
Sophia Jex Blake, an early British physician who became an active campaigner for the education of women, had to study in Berne, Switzerland, as she was unable to study for degrees in the UK. Another early female medic, Elizabeth Garrett Anderson - the first woman to openly qualify in Britain as a physician and surgeon, was awarded a degree in 1865, but soon after the Society of Apothecaries changed the rules preventing any more women registering to study.
In 1875, legislation was enacted allowing women to study medicine, however only some institutions actually allowed women to enrol, such as the Royal Free in London. It was only in 1944, four years before the creation of the NHS, that the government decided it would only provide funding for medical schools that admitted what it termed a ‘reasonable’ proportion of women - about one fifth.
We don’t actually know how many female doctors worked in the NHS when it was created. Data on gender in the workplace was not being collected and wouldn’t be deemed important for another 20 years. However, we do know two things. Women were a minority, and they often occupied lower levels in the professional hierarchy.
Some hospitals run for women by women existed in the NHS’ infancy but the vast majority of consultants in teaching hospitals were male.
Despite women working as doctors and nurses, there is some evidence that their professional status actually declined in the first few years of the NHS. During the war they had occupied the posts of men who were serving in the armed forces; when these men returned (along with others who had not previously worked in the NHS) they benefitted from programmes providing work and compensating for missing out on university education. These programmes often gave these men priority over women in employment.
Then came the post-war baby boom, with many women marrying returning servicemen and starting a family soon after. Unlike in some other countries, there were no legal restrictions on employment of married women at the creation of the NHS, however, for many years there was still a widespread belief that ‘a woman’s place was in the home’. Until 1970, women had to have a male guarantor to obtain a mortgage, and only in the 1960’s was safe contraception, controlled by women, widely available, along with access to legal abortion.
By 1965, women made up nearly 21% of all doctors on the medical register. Among those aged under 30 the percentage was slightly higher- almost 25%. By 1974, these figures had increased slightly but they were still a minority.
Today the situation is very different. In 2018, almost 46% of all doctors on the General Medical Council register are female, and those aged under 30 actually form a majority, at almost 57%.
The roles that women occupy have also changed. In the early days of the NHS, women were often found in posts offering part-time work, particularly community child health, pathology, and anaesthetics. Many also worked in general practice - sometimes in partnership with their husbands. Although women continue to be under-represented in some specialities, including surgery, the proportion of female trainees has increased greatly.
Women can now be found in senior roles across all medical specialities, with current examples including Professor Dame Sally Davies, Chief Medical Officer for England, Dame Jane Dacre, President of the Royal College of Physicians and Fiona Godlee, Editor in Chief of the British Medical Journal.
Despite this progress many barriers remain. Recent analyses demonstrate a significant under-representation of women in positions of leadership, including women holding 37% of senior leadership roles for clinicians on clinical commissioning groups and NHS provider boards, and among non-clinicians, only 12% are in lead roles. This underrepresentation is explained by the demands of childcare, male-dominated networks and outdated attitudes to women leaders.
In April 2018, the NHS reported a median gender gap in hourly pay of 17.4% while other sources cite it closer to 23% - importantly, these figures related to basic pay. In addition, female consultants were said to be 6.5 times less likely to receive the top clinical excellence awards - worth £77,000 a year.
Women have made an enormous contribution to the NHS throughout history. For most of that time their work was poorly recognised in a profession whose upper echelons was dominated by men. Even now, many women lack self-confidence, and are conditioned in traditional gender norms, thereby hampering their progress. This is changing, but there is no room for complacency.
This expert opinion piece is part of a series that LSHTM are publishing in the lead up to the 70th anniversary of the NHS on 5 July 2018. You can read more about our NHS 70 series and join the conversation online using #NHS70LSHTM.
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.