Global inequalities in survival for childhood leukaemia highlight need for better care
12 April 2017 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png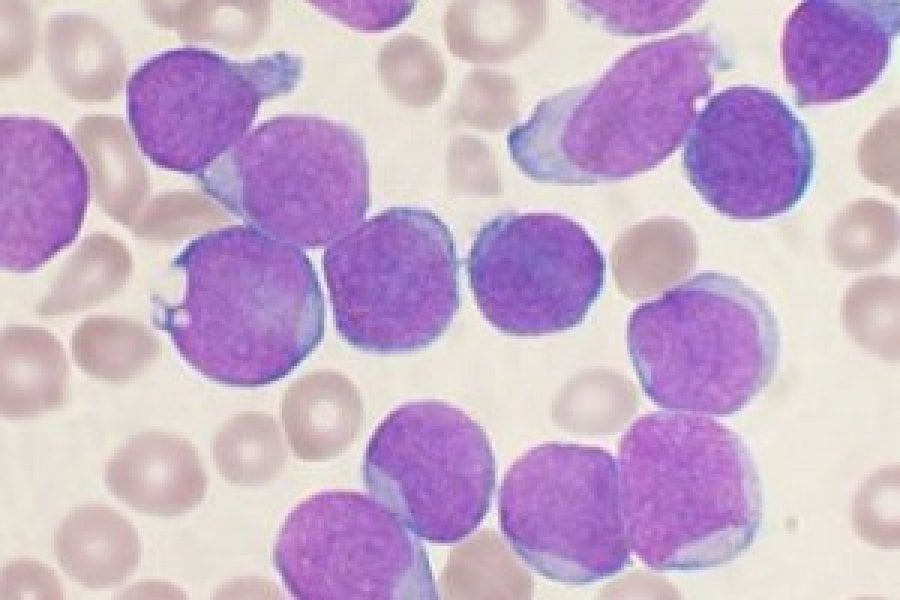
A Wright's stained bone marrow aspirate smear of patient with precursor B-cell acute lymphoblastic leukemia
Global inequalities in survival from childhood leukaemia have narrowed but they still persist, with five-year survival in some countries nearly twice as high as in others for children diagnosed during 2005-2009, according to new research published in The Lancet Haematology.
Led by the London School of Hygiene & Tropical Medicine, the study is the largest population-based comparison of survival from childhood leukaemia. It showed that while survival has increased in many countries, five-year survival for acute lymphoblastic leukaemia (ALL) in Germany was 92%, compared to 52% in Colombia for children diagnosed in 2005-2009. Additionally, the study highlighted that survival has improved for most age groups but remains lowest for infants under 1.
The authors used individual patient data for almost 90,000 children, provided by 198 cancer registries in 53 countries. They estimated survival for the two most common types of childhood leukaemia, acute lymphoblastic leukaemia (ALL) and acute myeloid leukaemia (AML), and for other less common blood cancers.
Taking into account the differences in age and the risk of death from other causes between countries and regions, the researchers found that five-year survival from childhood ALL and AML increased in most countries between 1995 and 2009. However, there were wide international inequalities.
Overall, ALL survival was the highest – with the probability of surviving at least five years ranging from 11% in China to 87% (Austria) for children diagnosed between 1995 and 1999. The range narrowed to 52% in Columbia and 92% in Germany for children diagnosed between 2005 and 2009.
There was significant progress in five-year survival for AML, but it remained lower than for ALL – increasing from between 4% in China and 72% in Sweden for those diagnosed between 1995 and 1999, to between 33% in Bulgaria and 78% in Germany for children diagnosed between 2005 to 2009. This is likely to be the result of recent improvements in diagnosis and treatment.
The authors highlight that in some countries, such as Germany and Austria, survival for ALL and AML has consistently been high compared to other nations, which might be due to closer adherence to treatment protocols.
Between 1995-1999 and 2005-2009, five-year survival for childhood ALL increased from 79% to 89% in the UK, and from 83% to 88% in the US. For AML, five-year survival increased from 59% to 68% in the UK and from 52% to 63% in the US. Survival in China increased substantially over the same period – from 11% to 69% for ALL survival, and 4% to 41% for AML survival.
The chances of survival depended on the child’s age when diagnosed with leukaemia. Overall, children aged 1-9 years old at diagnosis had higher survival for both types of leukaemia than those aged 10-14 years old or less than 1 year. Survival has improved for most age groups, for both ALL and AML, especially for children diagnosed with ALL aged 10-14 years. It is still lowest for children diagnosed in the first year of life.
Dr Audrey Bonaventure, lead author from the London School of Hygiene & Tropical Medicine, said: “There is room for improvement in the management of childhood leukaemia in many countries. These findings show the extent of worldwide inequalities in access to optimal health care for children with cancer. Survival for children with ALL can be as high as 90% at five years after diagnosis, and up to 80% for children with AML, but in some countries survival remains below 60% for both diseases.
“We do not yet know how to prevent leukaemia in children, but optimal treatment offers the chance of long-term survival for most children. Providing additional resources, alongside evidence-based initiatives such as international collaborations and treatment guidelines, could improve access to efficient treatment and care for all children with leukaemia. This would contribute substantially to reducing worldwide inequalities in survival.”
The study had limitations in some countries as a result of small numbers of patients and limited data collection. For example, in some low- and middle-income countries, the data were sparse, such that survival estimates could not be age-standardised, limiting the interpretation of survival trends.
Publication
Audrey Bonaventure, Rhea Harewood, Charles A Stiller, Gemma Gatta, Jacqueline Clavel, Daniela C Stefan, Helena Carreira, Devon Spika, Rafael Marcos-Gragera, Rafael Peris-Bonet, Marion Piñeros, Milena Sant, Claudia E Kuehni, Michael F G Murphy, Michel P Coleman, Claudia Allemani, and the CONCORD Working Group. Worldwide comparison of survival from childhood leukaemia for 1995–2009, by subtype, age, and sex (CONCORD-2): a population-based study of individual data for 89828 children from 198 registries in 53 countries. The Lancet Haematology.
Related links
Related courses
- Cancer Survival: Principles, Methods and Applications – short course
- Issues in Global Non-Communicable Diseases: from research to policy –short course
Image: A Wright's stained bone marrow aspirate smear of patient with precursor B-cell acute lymphoblastic leukemia. Credit: Wikicommons/Vashi Donsk
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.