Sexual health services need to be strengthened for PrEP users
3 January 2020 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png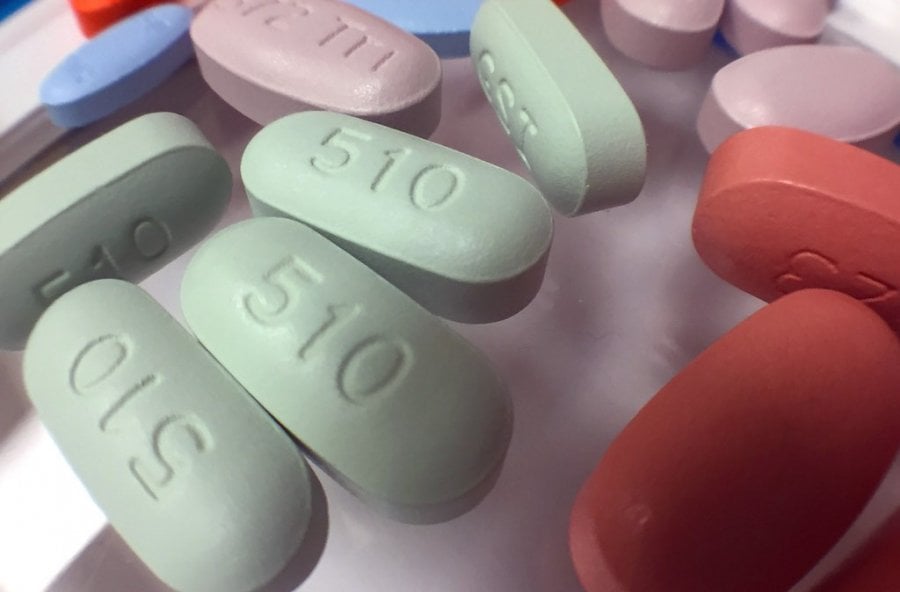
Antiretroviral drugs to treat HIV infection
However, a global study co-led by the London School of Hygiene & Tropical Medicine and Monash University in Australia, has shown that people who are seeking PrEP to prevent HIV are also at high risk of other sexually transmitted infections (STIs).
Supported by the World Health Organization, the study, published in JAMA Open Network, suggests PrEP services could be an ideal place to test for, prevent and treat both HIV and other STIs.
The review highlights the limited focus and investment in STI management within HIV programmes. It found that a quarter (24%) of people initiating PrEP were diagnosed with either chlamydia, gonorrhoea or syphilis before they started taking PrEP. Nearly three-quarters (72%) of those continuing to use PrEP were diagnosed with either chlamydia, gonorrhoea or syphilis within a year of starting PrEP.
The research team found that the same factors that place people at substantial risk for HIV, such as low condom use, barriers to accessing or using condoms and having more than one sexual partner, also increase their risk for acquiring other STIs.
Dr Jason Ong, co-lead author from the London School of Hygiene & Tropical Medicine and Monash University, said: “This global systematic review of the prevalence and incidence of STIs among users of pre-exposure prophylaxis for HIV identified 88 studies from 26 countries. We found a high prevalence of STIs in those starting PrEP, demonstrating that these programs are targeting high-risk individuals for HIV and other STIs, and high incidence of STIs in those persisting on PrEP. This underscores the need for ongoing sexual health services.
“HIV PrEP programs continue to be scaled-up globally. This offers an unprecedented opportunity to strengthen sexual health services through this growing infrastructure to high-risk populations that are now regularly engaged in our health system. PrEP programs can be a gateway to offer comprehensive sexual health care which should not only diagnose and treat STIs, but also offer vaccination, mental health support, substance use support and reproductive health services.”
PrEP consists of a combination of tenofovir and emtricitabine. It has been recommended for people at substantial HIV risk, such as men who have sex with men and people who inject drugs, by WHO since 2015.
Although most experience of PrEP implementation has been in high-income countries, PrEP services are now being developed for low- and middle-income countries. To date, more than 60 countries globally have national PrEP polices, including 20 in Africa.
Dr Rachel Baggaley from WHO’s Department for HIV, Hepatitis and Sexually Transmitted Infections, a co-author of the article said: “High numbers of curable STIs are being missed particularly in low- and middle-income countries. PrEP services can help prevent not just HIV but also STIs, and we should take advantage of this opportunity.”
Melbourne Sexual Health Centre Director Professor Christopher Fairley, said, “PrEP has the potential to be one of the most significant and powerful interventions to prevent HIV infection, and this paper has now highlighted an additional advantage of PrEP; that it provides an opportunity to improve the sexual health of those individuals and populations at highest risk of both HIV and STIs.”
Publication
Ong JJ et al. Global Epidemiologic Characteristics of Sexually Transmitted Infections Among Individuals Using Preexposure Prophylaxis for the Prevention of HIV Infection: A Systematic Review and Meta-analysis. JAMA Network Open. DOI:10.1001/jamanetworkopen.2019.17134
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.