TB cases and deaths predicted to spike due to COVID-19
24 June 2020 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png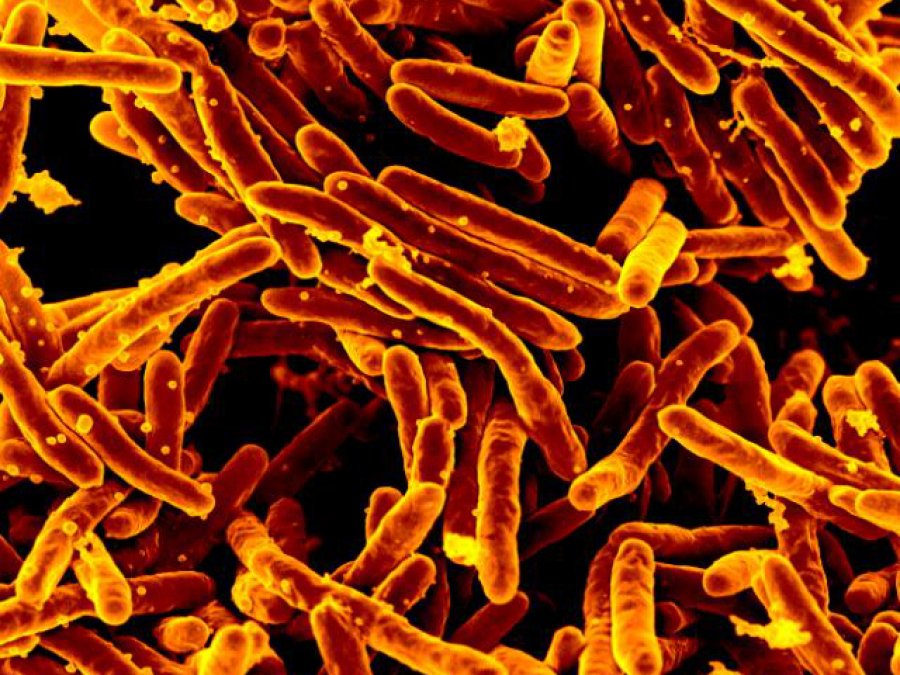
Mycobacterium tuberculosis MEB. Credit: NIAID on Flickr
The global COVID-19 pandemic could significantly increase the global burden of tuberculosis (TB) due to disruptions to health services, and delays to diagnosis and treatment, according to new estimates published in the European Respiratory Journal.
Before COVID-19, over 4,000 people were dying from TB every day. In countries where health services are strained, there is a fear that TB cases and deaths could rise significantly.
Researchers from the London School of Hygiene & Tropical Medicine (LSHTM) and Lancaster University estimated additional TB deaths and cases in China, India and South Africa over the next five years. They examined the impact of various reductions in social contacts and impacts on health services due to COVID-19.
The researchers hypothesised that social distancing might reduce TB incidence as Mycobacterium tuberculosis, the bacteria which causes the disease, is transmitted via droplets in the air – similar to the coronavirus.
However, even after taking into account this potential reduced TB transmission, the most likely scenario was estimated to result in more than 110,000 additional TB deaths.
In the worst case scenario where the impact of COVID-19 on health services is severe, this number could rise to up to 200,000 additional deaths.
First author Dr Finn McQuaid, Assistant Professor in Infectious Disease Epidemiology at LSHTM, said: “There is concern that the COVID-19 pandemic is resulting in decreased TB clinic attendance, delayed diagnosis and treatment. This is especially so in low- and middle-income countries where health services, or access to them, might be substantially disrupted. Early anecdotal information from China, India and South Africa suggests that the number of people being diagnosed and treated for TB has fallen significantly.”
The team measured the effect of these factors on TB incidence and deaths in China, India and South Africa, three countries which make up approximately 40% of the global TB cases. They modelled different scenarios with various implementations of social distancing measures and health service disruption lasting for six months to estimate the impact of COVID-19 on global TB burden.
They found that if there is substantial health service disruption, such as a 50% reduction in TB cases detected and successfully treated, there would be an increase in both incidence and deaths from TB over the subsequent five years, regardless of the level of social contact.
The most probable scenario, based on the current information and distancing measures, suggests 6,000 additional deaths could occur in China, 95,000 in India and 13,000 in South Africa.
However, if social distancing measures are minimal and there is substantial health care disruption – based on 80% reduction in case detection and treatment success – the model predicts an 8-14% increase in cumulative deaths from TB over the next five years.
Dr McQuaid explained: “We need to act now to ensure innovative approaches to people-centric TB care are the focus, so that the fight to end this pandemic doesn’t overwrite the hard-won gains made against this disease.
“Given that health service disruption far outweighs the benefit of social distancing, it is crucial to maintain and strengthen TB-related health services during, and after, COVID-19.
“It is also important to note that the decline of health services is likely to have a greater impact on drug-resistance TB patients, as they often require longer treatment. Additionally, we examined social distancing measures over a six month period, but with the potential of subsequent waves of the virus, the impact could last longer.”
The authors acknowledge limitations of their work including that it did not take into account setting-specific differences within the countries, while the effect on service delivery needs to be investigated in greater detail. It also did not incorporate external factors of the COVID-19 pandemic, including increased poverty or reduced access to antiretroviral treatments in areas of high HIV prevalence.
Further research is required to examine these factors, as well as whether TB patients are at higher risk of severe COVID-19.
Publication
C. Finn McQuaid, Nicky McCreesh, Jonathan M. Read, Tom Sumner, Rein M. G. J. Houben, Richard G. White, Rebecca C. Harris. The potential impact of COVID-19-related disruption on tuberculosis burden. European Respiratory Journal. DOI: 10.1183/13993003.01718-2020.
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.