COVID-19 vaccine refusal is higher among health and social care workers who feel pressured by their employers
12 May 2021 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png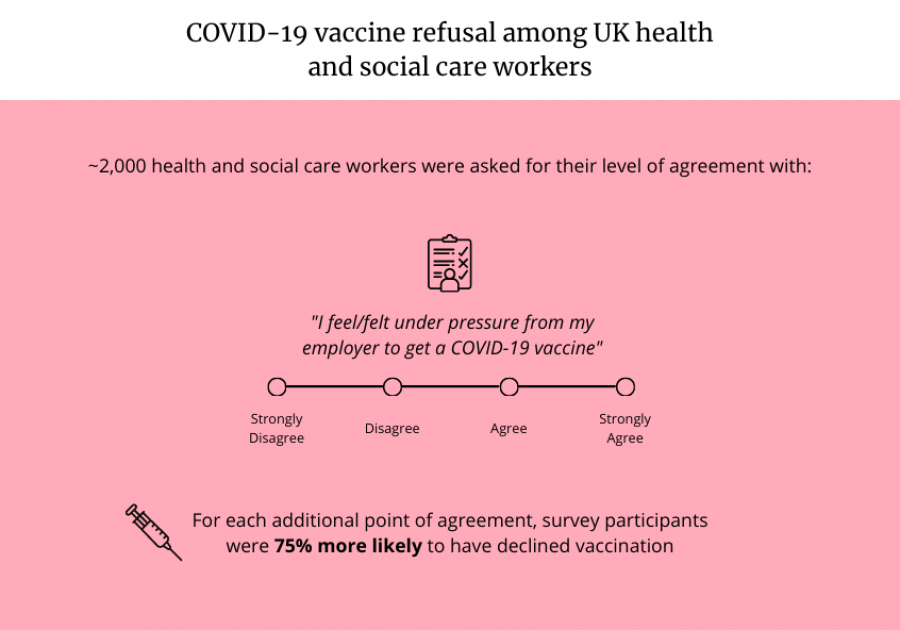
COVID-19 vaccine refusal among UK health & social care workers
Health and social care workers who felt under greater pressure from their employers to receive COVID-19 vaccination were more likely to decline it, according to preliminary new research highlighting factors influencing uptake.
The study, not yet peer reviewed, was led by the London School of Hygiene & Tropical Medicine (LSHTM) in collaboration with the NHS Race and Health Observatory, Public Health England and the Royal College of Nursing.
In a survey of nearly 2,000 people, participants were asked for their level of agreement with the statement ‘I feel/felt under pressure from my employer to get a COVID-19 vaccine’. This was asked on a 4-point scale from (1) strongly disagree to (4) strongly agree. For each additional point of agreement on the scale, participants were 75% more likely to have declined COVID-19 vaccination.
Amongst unvaccinated participants, worrying concerns were raised about how their vaccination decision might impact their job security. For social care workers, pressure was exacerbated by hearing of care sector employers making COVID-19 vaccination mandatory for staff, and the vulnerability of social care worker positions (e.g. employment on zero-hours contracts).
Feeling pressurised had damaging effects, eroding trust and negatively affecting relationships at work, and often exacerbated COVID-19 vaccination concerns and hardened stances on declining vaccination.
The study also identified structural barriers to vaccination uptake: Black African and Mixed Black African workers were not offered vaccination at the same rates as White British and White Irish participants (8.9% not offered as compared to 5.5%).
When additional demographic and situational factors were controlled for, Black African and Mixed Black African participants were around twice as likely not to be offered the vaccine as White British and White Irish participants, and social care workers were around 50% more likely to not be offered COVID-19 vaccination than health care workers. The latter, likely linked to the organisational structure and nature of roles within social care.
Dr Sadie Bell, Research Fellow at LSHTM and lead author said: “Our findings emphasise the importance of COVID-19 vaccination remaining voluntary. Organisational factors and workplace culture play an important role in the likelihood of both being offered and getting vaccinated. Health and social care providers need to offer a space for their staff to have “conversations” where they feel safe to ask about COVID-19 vaccination, and not feel judged and stigmatised for having questions and/or concerns.”
The research team used a mixed-methods approach – involving an online cross-sectional survey and interviews – to find out UK health and social care workers’ views on COVID-19 vaccination. 1,917 health and social care workers - 1658 healthcare workers (HCWs) and 261 social care workers (SCWs) - completed the survey. Twenty survey participants were interviewed.
1,102 participants (57.4%) were White British or White Irish, 94 (4.9%) were from other White backgrounds, 168 (8.8%) were Black African or Mixed Black African, 66 (3.4%) were Black Caribbean or Mixed Black Caribbean, 264 (13.8%) were from an Indian background, 109 (5.7%) were from a South-East Asian (including Pakistani and Bangladeshi) or Mixed Asian background and 90 (4.7%) were not categorised into any of the six ethnicity categories.
Participants who indicated stronger agreement with the statement ‘I would recommend my organisation as a place to work’ were more likely to have been offered COVID-19 vaccination. COVID-19 vaccination uptake was high amongst the survey participants, with 93.9% of health care workers and 90.0% of social care workers accepting the vaccination when offered.
Black African and Mixed Black African staff were almost twice as likely to decline a COVID-19 vaccine as White British and White Irish participants (9.5% and 5.1% respectively), citing reasons including concerns about a lack of research on COVID-19 vaccines and distrust in the vaccines, healthcare providers, and policymakers.
The survey revealed common reasons for declining the vaccine were concerns about side-effects and a lack of research on the vaccine. It revealed the main motivation for vaccine acceptance was protecting family members and friends, and self-protection from COVID-19.
Participants suggested tailoring vaccination communication to promote uptake amongst health and social care workers from ethnic minority backgrounds, and engaging faith leaders and trusted figures who understand community member concerns.
Sandra Mounier-Jack, an Associate Professor in Health Policy at LSHTM and study author, said: “Our work shows a move towards mandating COVID-19 vaccination is likely to harden stances and negatively affect trust in the vaccination, provider, and policymakers. Health and social care employers are in a pivotal position to facilitate COVID-19 vaccination access, ensuring staff are aware of how to get vaccinated and promoting a workplace environment in which vaccination decisions are informed and voluntary.”
The authors acknowledged limitations of their study, including survey recruitment from social media and professional bodies – which intentionally aimed at over-sampling ethnic minority groups – may have led to some ethnic or professional groups being over- or under represented compared to the overall demographics of the UK health and social care worker population.
The National Institute for Health Research (NIHR) funded this study as part of the Health Protection Research Unit in Vaccines and Immunisation. The Health Protection Research Unit in Vaccines and Immunisation is a research partnership between the London School of Hygiene & Tropical Medicine and Public Health England, in collaboration with the University of Cambridge.
Publication
Sadie Bell, Richard M Clarke, Sharif A Ismail, Oyinkansola Ojo-Aromokudu, Habib Naqvi3, Yvonne Coghill, Helen Donovan, Louise Letley, Pauline Paterson, Sandra Mounier-Jack. COVID-19 vaccination beliefs, attitudes, and behaviours among health and social care workers in the UK: a mixed-methods study. MedRxiv pre-print.
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.