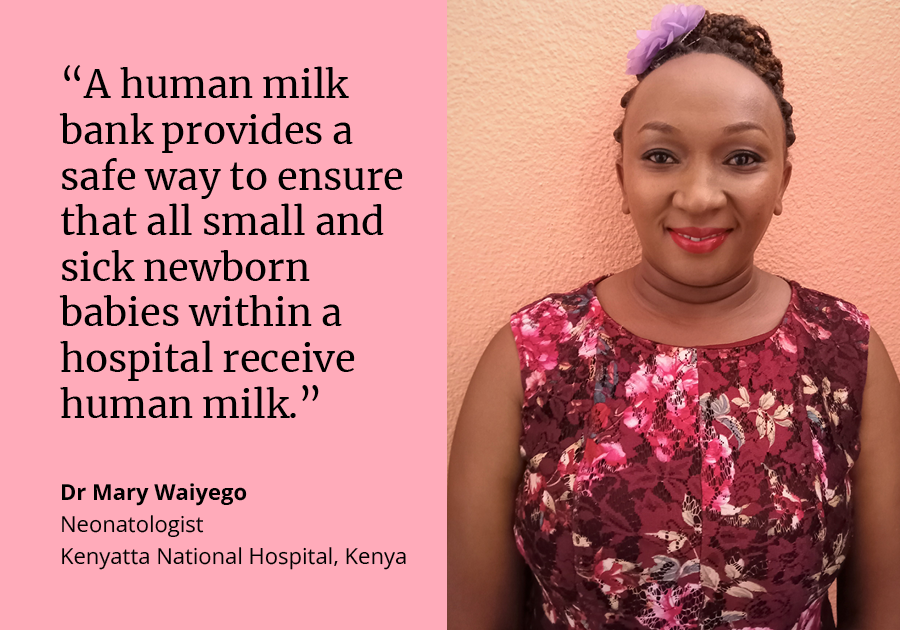
World Breastfeeding Week: An interview with neonatologist Dr Mary Waiyego
3 August 2023 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.pngThe World Health Organization (WHO) recommend that babies begin breastfeeding within one hour of birth and are exclusively breastfed for the first six months of life, yet nearly two out of three infants globally are not. World Breastfeeding Week raises awareness of the benefits of human breast milk and promotes breastfeeding education and support.
In 2020, Kenya had a neonatal mortality rate of 21 per 1,000 live births. Dr Mary Waiyego is a neonatologist at Kenyatta National Hospital in Nairobi, Kenya. She shares her experience working in Kenya’s first human milk bank at Pumwani Maternity Hospital, Nairobi, including the impacts on newborn health and challenges faced.
Why is human milk important for small and sick newborns?
For healthy newborns, human breast milk has optimal nutrition content in terms of calories and nutrients, it is an essential source of energy. It also comes with immune properties, protecting babies from infections and reducing newborn mortality. Babies will get sick less if they are fed on breast milk. For preterm babies, human milk is also digested more easily compared to formula.
Alongside this, unlike formula milk which needs to be purchased, human milk is freely available and doesn't require any mixing, so it doesn’t require safe clean water to be used for reconstitution.
What is a human milk bank?
The World Health Organization (WHO) recommends that all newborns should receive human milk and that breastfeeding should be supported and promoted so that every mother is encouraged to breastfeed her own baby. However, there are some circumstances where the mother may not be able to provide her own breast milk to her baby for example due to illness or death, or if the baby is unable to latch to her breast properly.
A human milk bank provides a safe way to ensure that all small and sick newborn babies within the hospital receive human milk. It collects, processes and distributes milk to newborns in need. It also ensures that mothers who have excess milk, over and above what their own babies require, have somewhere where that milk is collected.
Can any new mother donate to a milk bank?
It depends on the policies of the milk bank, most banks worldwide get milk from any screened lactating mother within the hospital who has extra milk to donate. It’s a voluntary process. There are some regions that have milk collection centres, outside the hospital, that people can donate milk to. The milk is stored in the right conditions and then transported to the central processing milk bank for distribution.
The milk bank at Pumwani Hospital in Kenya only operates within the confines of the hospital. There is no system in place yet that allows for collection from the community or distribution of milk to babies outside the hospital. It gets milk from admitted mothers and it gives the milk to the admitted babies.
Is collecting and distributing milk outside the hospital something that the Kenya milk bank will do in the future?
Yes, in the future there should be a system like this because there are a lot of mothers out there who are willing and have extra milk to donate and many babies who need it.
Some people have a negative view of milk banks as they think they may discourage mothers from working towards breastfeeding their own babies. However, there are studies that have shown that mothers who are supported in the initial days, when they're struggling to provide milk, actually end up exclusively breastfeeding later down the line, often more than those who do not get that initial support.
A human milk bank comes hand in hand with other activities geared towards supporting and promoting breastfeeding. This includes assisting mothers to get established with latching and supporting them to produce enough supplies. But despite these efforts sometimes mothers will be unable to produce the volumes that their baby needs, so that's where the donated human milk comes in.
What other activities are there to support these mothers in the first few weeks after birth?
Ideally, support for breastfeeding should start from the beginning of an expectant mother’s journey so during their antenatal visits, the clinicians or the nurses or the health workers looking after them, should explain the importance of being ready to exclusively breastfeed. They should assess the breasts for any problems so that those are captured early. During delivery, they should ensure that arrangements are made for the baby to get their first colostrum (the first form of breastmilk released after giving birth).
The health workers will also support the new mother to have skin to skin contact with their newborn immediately after birth. If a baby is born healthy, they will ensure that they're not separated from the mother by rooming-in (keeping the newborn in a crib at the mother’s bedside).
New mothers are assisted with the techniques of expressing milk, latching on the breast, positioning, and are given information on the frequency of expressing and what needs to happen for a successful breastfeeding experience. That's in addition to making sure that their health is looked after, any pain is controlled, and that they get proper nutrition. All these activities are aimed at encouraging mothers to achieve full breastfeeding or at least expressing milk to feed their baby.
How do you decide what newborns get the donated milk?
There are two sets of babies: healthy and small and sick. If there is an abundance of milk in the hospital, every baby, healthy or not, can receive donated human milk, provided that the parents are made aware and consent, or a guardian or clinician consents if a parent is absent. We have criteria that determines who receives the milk first, but our priority would always be the small and sick newborns. If supply is not a problem, then any baby can receive donor human milk.
Was the milk bank in Kenya affected by COVID-19?
Not to a large extent. Generally, the number of patients in the hospital reduced, which impacted the number of people donating. However, the mothers who did come in and had no COVID-19 symptoms were encouraged to express their milk and donate. The screening process was quickly adjusted so that mothers who had COVID-19 symptoms could not interact in close range with other mothers. Mothers underwent screening for COVID symptoms. Only those who had a negative test were allowed to access the milk bank.
While you were working at the milk bank, what were the key gaps or needs?
I left the milk bank several years ago so I may not know their current needs, but I can talk about the gaps while I was there.
It would be great to have a system that allows for more donors, because sometimes we would run out of milk and be unable to provide the maximum support for the babies within the hospital. Our work would be easier if we had an automated system with updated registers and digital records that show the availability of human milk at the click of a button.
Then we need a very efficient lab support system. The backbone of a milk bank is safety – we need to guarantee the milk is safe to use and we rely on the laboratory support to do this quickly and effectively.
The other thing I would have wanted is to be able to cater for a bigger mission, because while I worked there, we had a lot of external calls for support. During the Delta wave of COVID-19, mothers were giving birth early and, in some cases, dying. Preterm babies are very small and cannot cope with formula milk, but while I was there, there was no system to provide milk to other newborns outside the hospital. This is a system that can only be developed by the national government, because it is an investment and there are a lot of resources and logistics involved.
Finally, there is the issue that there are few manufacturers producing the equipment we used so there were no local support teams that could help if something went wrong. It involved a lot of back and forth on the phone troubleshooting.
These are some of the gaps from when I worked there but things may have changed since.
What other impacts have you seen because of the milk bank?
The consumption of formula milk within the hospital reduced which had a knock-on effect on the amount of money being spent on formula. Establishing a human milk bank is an investment because the infrastructure has to be right, the equipment needs to be purchased and training given on safety and processing. But it is a cost-effective investment compared to the recurring expenditures for formula and the benefits of human milk
There are ongoing costs in a milk bank such as for the laboratory reagents and cleaning the reusable bottles, but savings are made by reducing the duration of hospital stays and increasing the number of babies on full milk, as opposed to intravenous fluids. Every extra day a baby stays in hospital there are costs so cutting these down results in savings.
Why is World Breastfeeding Week important?
As a neonatologist, World Breastfeeding Week is of great importance because in addition to healthy babies, we also take care of very sick and very tiny newborns. These newborns don't have many options in terms of what they can ingest so ensuring that we give them the optimal nutrition for their growth and development, to avoid complications and even death, is very important to me.
Working with mothers is a partnership and engagement with them to take care of the needs of their babies is of great importance to me. I have seen the devastating effects of some of the complications that babies can get when they don't receive breast milk - it can be a disaster. But this could easily be averted by simply giving the babies what they need to get in terms of nutrition.
World Breastfeeding Week is important because it raises awareness for people who may not know or understand the importance of human milk for babies. Some may think that it's a choice that you can very easily make without knowing how important it is to make sure that every baby gets human milk. It's important that this is observed so more awareness is created and more people take responsibility.
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.