The impact of war on maternal health: reports from Gaza
10 March 2025 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png
1. Your research focuses on the impact of the war in Gaza on maternal health. What initially led you to explore this issue?
As an epidemiologist specialising in both maternal and child health as well as nutrition, I was initially establishing a birth-to-education cohort of Palestinian refugees. My work examined various maternal and newborn health outcomes, including C-section rates and post-term deliveries. However, the war in Gaza and Israel’s attacks on healthcare facilities compelled me to shift my research focus. My goal became twofold: to assess the immediate effects of the war on maternal and newborn health, and to inform humanitarian responses and accountability efforts.
2. From what we know so far, how has the crisis affected access to care for pregnant women and new mothers?
The war has drastically altered maternal care in Gaza. Our analysis of where women were giving birth before and after 7 October 2023 showed a shift from government hospitals towards NGO hospitals as many facilities became damaged and inaccessible. While our full report is still under peer review, the preliminary findings are concerning: C-section rates dropped, while preterm births increased. We also documented a severe reduction in post-delivery hospital stays, with mothers and newborns discharged dangerously early due to overcrowding and safety concerns. Right now, emergency obstetric care is available in just a fraction of healthcare facilities that existed before the war, creating dangerous conditions for women experiencing complications during childbirth.
3. What are some of the key challenges facing healthcare providers working in maternal and newborn care in Gaza today?
Beyond the destruction of healthcare facilities and severe supply shortages, healthcare providers are struggling with winter conditions. Reports suggest a rise in preventable newborn deaths due to insufficient heating. Essential medications like oxytocin, magnesium sulfate and antibiotics are scarce. UNRWA, the primary UN agency providing humanitarian assistance to Palestinian refugees, has historically provided most pregnancy-related services in Gaza and continues to operate. However, recent political threats to its funding and access to Palestine raise serious concerns about the future of maternal and newborn healthcare services.
4. Your research is looking into both direct and indirect causes of maternal deaths in conflict settings. Can you share some insights into how these factors interact in a crisis like Gaza?
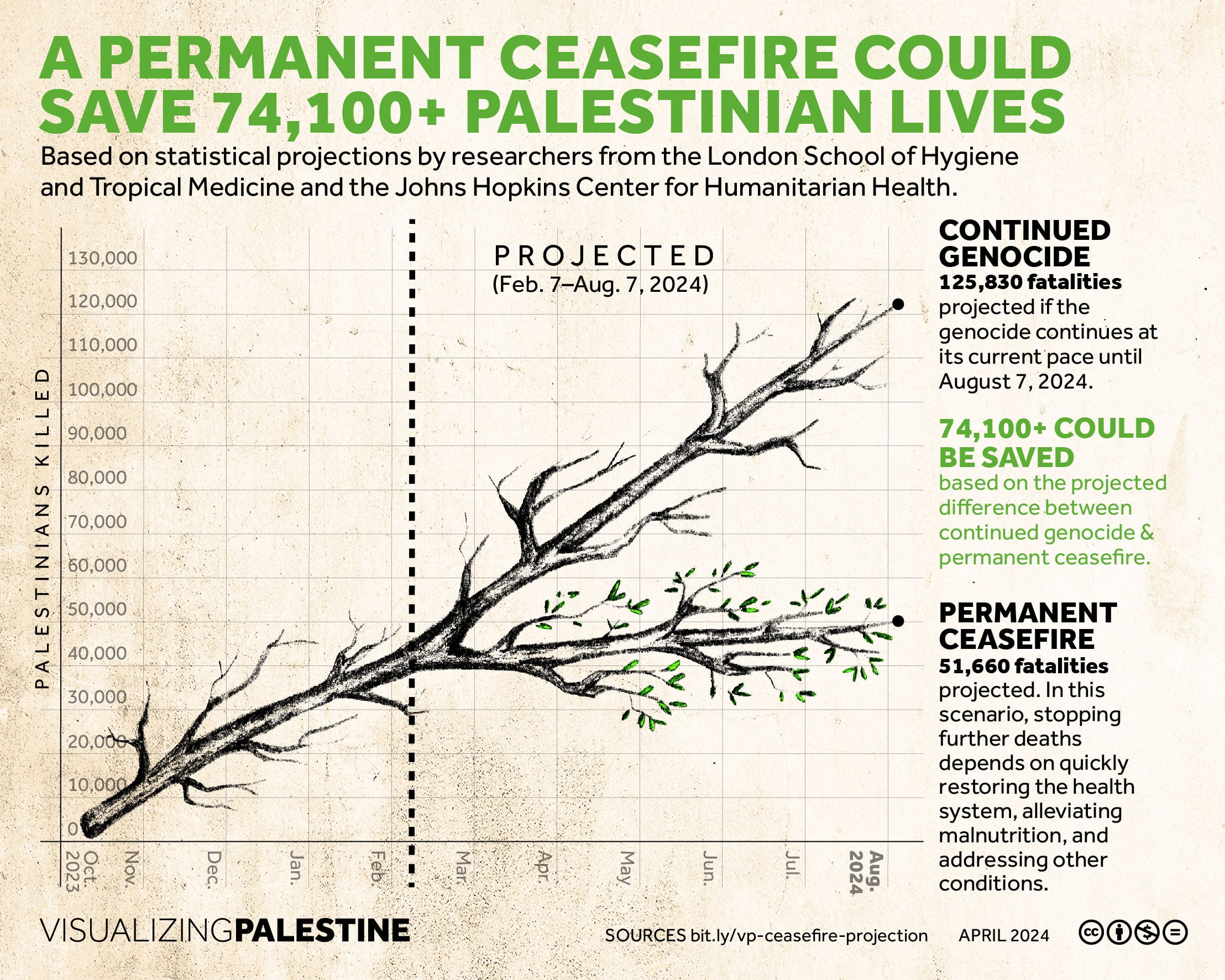
Direct trauma from the war is the most immediate threat to maternal and newborn life. However, indirect factors like disruptions in healthcare access, increased food insecurity, and declining water quality have devastating effects. Our projections of maternal death rates under different scenarios (ceasefire, status quo, escalation) suggest these indirect factors could reverse decades of progress, potentially pushing Gaza’s maternal mortality rates back to levels seen 30 years ago.
5. Given what we already know from past conflicts, what patterns are emerging in terms of maternal health risks?
Past conflicts have shown that maternal mortality, stillbirths, and neonatal deaths typically rise. Our findings in Gaza confirm this pattern, but Gaza stands out amongst other documented maternal mortality in conflict settings. The number of pregnancy-related deaths has exceeded patterns seen in other war zones. This happened because of several factors coming together – direct attacks on hospitals and clinics, the constant bombing making it unsafe for women to travel to get care, the prolonged siege cutting off medical supplies, and mass forced displacement. All of this really highlights why we urgently need international enforcement of humanitarian protections for women in conflict affected settings.
6. How are healthcare workers and humanitarian organisations adapting to the deteriorating conditions to continue providing maternal care?
Healthcare workers were forced to move maternal services out of bombed, damaged or inaccessible hospitals into field hospitals. The situation was quite desperate – medical teams performed surgeries by headlights during power outages. Preventable infant deaths occurred because incubators failed when electricity and fuel ran out. The medical shortages put doctors in impossible situations – they had to perform C-sections without proper anaesthesia, and in cases where women haemorrhaged after birth, doctors sometimes had to remove the uterus entirely because blood transfusions simply weren't available.
7. What are the broader implications of your research for maternal health?
Our research shows how quickly maternal health systems can collapse in war. Our findings have supported advocacy efforts for a ceasefire while also documenting violations of reproductive health rights for accountability efforts. This documentation helps establish patterns of harm that might later be used in formal investigations, ensuring that attacks on maternal healthcare aren't forgotten or normalised as simply "collateral damage" of conflict.
8. How do you hope these findings will inform humanitarian responses and policy decisions?
By combining projection models with real-time data, we are identifying key factors that are affecting maternal health and survival in Gaza, helping humanitarian actors to prioritise interventions. We are simply calling for the protection of fundamental human rights—ensuring healthcare facilities remain operational, safeguarding access to care, and providing essentials like food, water, electricity, and medical supplies. These are not extraordinary demands but the bare minimum for human dignity and life.
9. Looking ahead, what further research is needed to ensure better maternal health outcomes in crisis settings?
Our next research will explore the effects of conflict on Palestinian refugee children’s wellbeing and future potential. By integrating electronic health cohort data with geolocated and time-stamped conflict data, we aim to assess how conflict exposure impacts healthcare and education service utilisation and maternal, child health, nutrition, and education outcomes. This research will increase our understanding of conflict’s long-term effects and help develop more effective and targeted response strategies. Additionally, there is an urgent need to improve data collection in war zones and evaluate interventions such as mobile clinics, community programs, and telehealth to ensure access to quality maternal healthcare services.
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.