We aim to address the urgent need for improving control of non-communicable diseases in West Africa, where healthcare has been traditionally neglected and driven by disease-specific programmes, with limited engagement of local communities.
Our partnership is led by the London School of Hygiene and Tropical Medicine (LSHTM) and Ghana College of Physicians and Surgeons (GCPS), and involves Ashesi University (AU), Laboratoire d'Etudes et de Recherche sur les Dynamiques Sociales et le Développement Local [Research Laboratory on Social Dynamics and Local Development] (LASDEL) and Université Catholique de l'Afrique de l'Ouest - Unité Universitaire at Bobo-Dioulasso [Catholic University of West Africa - University Unit at Bobo-Dioulasso] (UCAO-UUB).
The NIHR Global Health Research Centre for non-communicable diseases in West Africa is part of the NIHR and hosted by LSHTM and GCPS.
Funded by the National Institute for Health and Care Research (NIHR), between 2022 and 2027, the NIHR Global Health Research Centre for Non-communicable Disease Control in West Africa (Stop-NCD) project is a partnership between the Ghana College of Physicians and Surgeons, the London School of Hygiene & Tropical Medicine, Ashesi University, Laboratoire d'Etudes et de Recherche sur les Dynamiques Sociales et le Développement Local [Research Laboratory on Social Dynamics and Local Development] (LASDEL) and Université Catholique de l'Afrique de l'Ouest - Unité Universitaire at Bobo-Dioulasso [Catholic University of West Africa - University Unit at Bobo-Dioulasso] (UCAO-UUB). We will use comprehensive and sustainable approaches to capacity strengthening, improving individual, organisational and system-level capacities of:
- researchers, particularly earlier-career staff, for high-quality applied NCD research,
- local communities, to engage with and improve behaviours and decisions affecting their health and
- policymakers and practitioners, to implement evidence-based NCD interventions.
We aim to improve health and wellbeing of populations in West Africa by developing capacity for high-quality research to inform improved prevention, diagnosis and treatment of inter-connected NCDs (hypertension, diabetes and co-existing stress, anxiety and depression).
To do this we will:
- Work in three West African countries (Ghana, Burkina Faso and Niger) with varying ethnic, social, cultural and economic environments to develop, implement and evaluate ways of improving control of hypertension, diabetes and related stress, anxiety and depression.
- We will start by analysing roles of key stakeholders (patients and communities, health workers, managers, policymakers) in the development, provision and use of NCD policies, programmes and services in each country, using appropriate methods such as analysis of available data, observations and interviews;
- Working closely with those stakeholders, we will co-produce packages of interventions for improving NCD control. This package will include adapting international guidelines to local contexts and supporting healthcare workers in implementing these, and establishing a community-based prevention, early-detection and management of NCDs;
- We will implement and rigorously evaluate the interventions packages for their costs and effectiveness, assess their potential for wide-scale application, and will identify transferable lessons for improving NCD control beyond these three countries.
Throughout these steps, we will:
- strengthen individual skills and expertise, organisational systems and processes and system-wide networking capabilities and leadership of: researchers (to conduct high-quality research), local communities (to engage with, and understand, how to enable healthy lifestyles) and policymakers and practitioners (to implement evidence-based NCD interventions);
- engage with key stakeholders (patients, health workers, managers) for consulting on their views, preferences and expectations, sharing results as they emerge and facilitating uptake of research results into their decisions and practices;
- maintain equitable international partnerships, through shared leadership involving both senior and earlier-career staff
London School of Hygiene & Tropical Medicine (joint lead organisation)
- Prof Tolib Mirzoev
- Prof Martin McKee
- Prof Dina Balabanova
- Prof Pablo Perel
- Dr Eleanor Hutchinson
- Dr Neil Spicer
- Dr Adrianna Murphy
- Dr Yasmin Jahan
- Miss Veronika Reichenberger
- Miss Linnet Griffith-Jones
- Ayan Aden Hag Hersi
Website: www.lshtm.ac.uk
Ghana College of Physicians and Surgeons (joint lead organisation)
- Prof Irene Agyepong
- Prof Evelyn Ansah
- Dr Abraham Oduro
- Dr Mary Amoakoh Coleman
- Dr Jacob Nonvignon
- Dr Augustina Koduah
- Dr Edward Antwi
- Dr Abigail Nyarko Codjoe Derkyi Kwarteng
- Prof Sammy Ohene
- Dr Henry Lawson
- Dr James Akazili
- Ms Linda Lucy Yevoo
- Dr Elizabeth Awini
- Prof Benjamin Uzochukwu
- Dr Annick Tiemele
- Ms Nana Efua Enyimayew
- Ms Grace Aye
- Mr Samuel Ayisi
- Dr Abraham Hodgson
- Dr Eric Odei
- Dr Leveana Gyimah
- Dr Keziah Naa Amerley Akosua Amarteyfio
- Dr Nyhira Yaw Adjei-Banuah
- Dr Eugene Paa Kofi Bondzie
- Dr Roberta Naa Barkey Ayiku
- Dr Dominic Anaseba
- Mr Labram Massawudu Musah
- Dr Abdul-Basit Abdul-Samed
Website: gcps.edu.gh
Ashesi University
- Prof Angela Owusu Ansah
- Dr Elena Rosca
- Mr William Ohene Annoh
- Dr Esther Laryea
- Dr Danyuo Yiporo
- Mr David Sampah
- Mr David Sasu
Website: www.ashesi.edu.gh
Laboratoire d'Etudes et de Recherche sur les Dynamiques Sociales et le Développement Local [Research Laboratory on Social Dynamics and Local Development] (LASDEL), Niger
- Prof Aissa Diarra
- Prof Jean Pierre Olivier de Sardan
- Dr Nassirou Ibrahim
- Dr Oumarou Saidou
- Mr Siddo Moumouni
- Ms Aissatou B Sow
- Ms Fatoumata Almahai
- Ms Salamatou Yamba
- Mr, Téoma M. Ousseini
- Mr Farouck Gaoh
- Dr Abdoulaye Ousseini
Website: lasdel.net
Université Catholique de l'Afrique de l'Ouest - Unité Universitaire at Bobo-Dioulasso [Catholic University of West Africa - University Unit at Bobo-Dioulasso] (UCAO-UUB), Burkina Faso
- Dr Maurice Yaogo
- Dr Paolo Ferraris
- Prof Clement Ziemlé Meda
- Dr Vincent-Paul Sanon
- Dr Anicet Touwendsida Kaboré
- Dr Jean Paulin Ki
- Dr Ange Nkokolo Massamba
- Dr Blahima Konaté
- Dr Emilie Pigeao-Gagné
- Dr Jean-André Ki
- Mr Ludovic Deo Gracias Tapsoba
- Mr Yamba Kafando
- Mr Souleymane Kékélé
- Miss Korotime Traoré
- Miss Sana Lisata
- Miss Zagre Cynthia
- Miss Diallo Rasmata
- Mr Simon Konkobo
- Mme Geneviève Ouedraogo
- Miss N’Charick Mafinè Ouattara
Website: ucao-uub.com
The NIHR Global Health Research Centre for non-communicable diseases in West Africa is part of the NIHR and hosted by LSHTM and GCPS.
We are committed to embedding our work in the contexts we are working in though working closely with stakeholders at all levels of the heath and research systems.
The Centre’s goal is to contribute to improved health of West African populations through comprehensive and sustainable capacity strengthening for high-quality applied NCD research to improve prevention, diagnosis and management of hypertension, diabetes and related common mental disorders (anxiety, stress, depression). Our ambition is to leave a legacy of person-centred, integrated (not disease-specific) and system-wide (combining staff, structures, resources at multiple levels) responses to inter-connected NCDs at community and primary care levels, through African-led research by high-calibre scholars embedded within supportive institutions, networks and policy environments, all ultimately contributing to reduction in premature mortality from NCDs, improved health, wellbeing and socio-economic benefits.
We will develop generalisable theoretical and practical lessons for effective NCD control and capacity strengthening, through working across diverse language-institutional-socio-economic contexts of Anglophone (Ghana, lower-middle-income) and Francophone (Niger and Burkina Faso, low-income) countries, identified based on their capacity and research needs, and strong academic/policy/community partnerships.
Our objectives are to:
- Deepen understanding of contextual influences and effective pathways to prevention, diagnosis and management of NCDs in West Africa;
- Co-produce with key stakeholders, contextually-adapted packages of interventions for prevention, diagnosis and management of NCDs at community and primary care levels; and conduct formative process evaluation;
- Implement the intervention package through existing health systems in each country, and evaluate its feasibility, acceptability, clinical effects, equitable reach and cost-effectiveness;
- Comprehensively and sustainably strengthen capacities of researchers, communities and decision-makers, for high-quality applied NCD research and its uptake;
- Ensure effective research communication and uptake into policies and practices of patients, communities, service providers, and national/West African decision-makers;
- Continuously engage with key stakeholders at community, sub-national, national levels within each country and within West Africa;
- Establish and maintain equitable partnerships between the West African and UK applicants, through shared leadership and governance arrangements
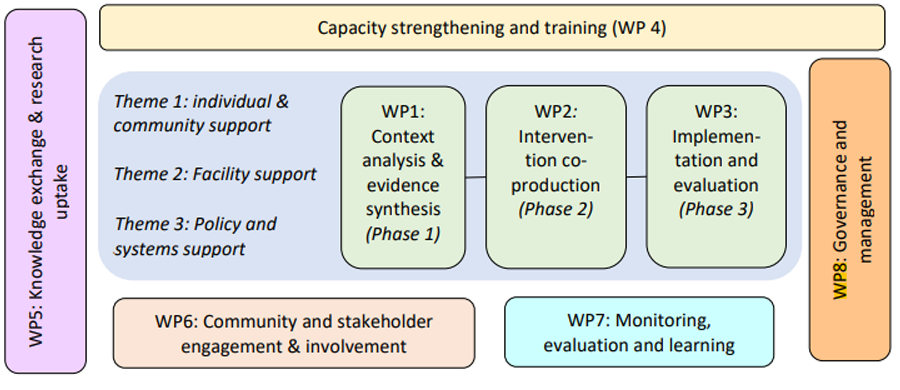
To meet our objectives we will structure activities in eight work packages:
- WP1: Context analysis and evidence synthesis
-
Work package 1 includes: stakeholder analysis and comprehensive analyses of socio-political-cultural-economic contexts of provision and use of NCD services at system, community, household and individual levels, using secondary data analysis, observations and in-depth interviews and a systematic review with a provisional question “which interventions can ensure person-centred, integrated and system-wide responses to inter-connected NCDs in West Africa?”
- WP2: Intervention co-production
-
Work package 2 involves working closely through regular meetings with key stakeholders, including patients, communities, service providers, managers and policymakers, to co-produce context-adapted packages of interventions. We will use our experience in co-production and participatory action research in engaging stakeholders as co-researchers throughout four-step action research cycles, to avoid a ‘travelling model’ approach where effective interventions are carried inappropriately across settings.
- WP3: Implementation and evaluation
-
WP3 focuses on implementation and evaluation of intervention packages. Implementation will be through local structures and processes, to ensure sustainability and we will evaluate feasibility, acceptability, clinical effects, equitable reach, and cost-effectiveness of the interventions packages.
Evaluation of the intervention packages will comprise: formative, using observations, interviews, analysis of service data and documentary analyses; seeking to refine the co-produced intervention packages, and summative quasi-experimental stepped wedge study design, combining analyses of routine service data, periodic household surveys, interviews, focus groups, observations and document reviews.
- WP4: Capacity strengthening and training
-
Work package 4 will target individual, organisational and system-level capacities of researchers, particularly earlier-career staff, and their organisations, for high-quality applied NCD research; communities, to engage and improve behaviours and decisions affecting their health and policymakers and practitioners, to implement evidence-based NCD interventions.
- WP5: Community and stakeholder engagement and involvement
-
Work package 5 will see engagement with communities and stakeholders through regular meetings for co-producing, implementing and evaluating interventions and research uptake. We will establish country-specific multi-stakeholder forums informed by stakeholder analysis to extensively consult with, and ensure representation of neglected community voices in NCD research.
- WP6: Knowledge exchange and research uptake
-
Work package 6 will see the development and implementation of a knowledge exchange and research uptake strategy. This strategy will inform mapping of knowledge preferences and expectations by different stakeholders including communities, practitioners, policymakers as part of the initial analyses and capacity assessments.
- WP7: Monitoring, evaluation and learning
-
Work package 7 will see the development and implementation of a comprehensive monitoring evaluation and learning strategy capturing key milestones to reflect the three research phases. We will use metrics for equitable partnerships, research, capacity strengthening and overall impact in our approach to knowledge exchange.
- WP8 Governance and management
-
Work Package 8 will ensure excellent coordination of the centre, through the development of appropriate, and equitable governance and management arrangements to support the aims of the centre are met and to support continuous communication with the partners and the funder and other key stakeholders.
Our three research themes reflect the level of support for person-centred, integrated and system-wide responses to interconnected NCDs through:
- Individual and community support
- Primary healthcare facility support
- Systems and policy support
Research themes are interrelated, build on, and complement, each other. For example, individual awareness about the nature and importance of NCD risk factors affects health seeking behaviours. Facility-based care is contingent on support for staff and an enabling policy environment.
Work within each theme is organized according to our three research workpackages: context analysis and evidence synthesis intervention co-production and implementation and evaluation Each theme has research questions, to be addressed through country-specific research projects, which will organise resources for generation of evidence.
Our goal is to contribute to improved health and wellbeing of populations in West Africa, through comprehensive and sustainable capacity strengthening for high-quality applied NCD research to inform improved prevention, screening, primary care diagnosis and management/referrals of interrelated hypertension, diabetes and common mental health problems. Our ambition is to leave a legacy of excellent African-led NCD research by high-calibre researchers embedded within supportive institutions and networks, which will contribute to improved health outcomes, wellbeing and wider socio-cultural-economic benefits in West Africa.
Our approach to community engagement and involvement is underpinned by a commitment to transformative engagements with individuals and groups throughout mutually-respectful, inclusive and ethical research. Transformation can take place when the knowledge and experiences of marginalised populations are articulated, understood, and centred within the research; when knowledge-based power is redistributed and mutual learning is centred. We will ensure these through participatory co-production using action-reflection cycles. This will allow our in-depth understanding of the intersecting experiences of marginalisation and exclusion, and enable communities to identify and articulate their needs for information to solve what they perceive as key issues in addressing the inter-related NCDs. The local communities are diverse, and we will be attentive to the power dynamics of these groups.
In each country, we will establish an in-country multi-stakeholder forums comprising 15-20 decision-makers, health workers, managers and practitioners, and civil society organisations. These advisory bodies will also help represent all voices in NCD research and provide platform for cross-stakeholder exchange, engagement, advocacy and joint decision-making.
Central to our plans is engaging and involving people living with NCDs, their families and carers, including those often marginalized. We will support, train and strengthen capacity of people living with NCDs to get involved in the NCD research and control. This will be done through close partnerships with, and supporting the work of, all above-mentioned CSOs working in their respective languages and within relevant social contexts. The rationale for this approach is to build on and extend existing processes and networks rather than create new, and potentially less sustainable, channels.
Our CEI activities will directly shape research to ensure its impact. We will particularly identify, and adapt where feasible, creative approaches to CEI such as photovoice, participatory film-making, local theatres. The continued cross-country peer-exchange, support and sharing will enable mutual learning and maximising impact for the benefit of the local people and communities.
Our goal is to contribute to improved health and wellbeing of populations in West Africa, through comprehensive and sustainable capacity strengthening for high-quality applied NCD research to inform improved prevention, screening, primary care diagnosis and management/referrals of interrelated hypertension, diabetes and common mental health problems. Our ambition is to leave a legacy of excellent African-led NCD research by high-calibre researchers embedded within supportive
institutions and networks, which will contribute to improved health outcomes, wellbeing and wider socio-cultural-economic benefits in West Africa.
We will use comprehensive and sustainable approaches to capacity strengthening, improving individual, organisational and system-level capacities of: (a) researchers, particularly earlier-career staff, for high-quality applied NCD research, (b) local communities, to engage with and improve behaviours and decisions affecting their health and (c) policymakers and practitioners, to implement evidence-based NCD interventions. This will be achieved through a combination of post-graduate training, short courses and workshops, structured mentorship support, cross-organisational exchange and learning, communities of practice and the co-production process itself.