This article first appeared on Mosaic and is republished here under a Creative Commons licence. As the article is not part of LSHTM’s feature series, please refer to Mosaic for republishing guidelines.
We now know there’s a cheap, safe treatment that could save thousands of lives each year. But those who need it can’t always access it.
Twenty-eight weeks into her first pregnancy, Rabia’s worst fears were realised. She went into labour, and the baby was stillborn. The bleeding started the next day.
“It was severe bleeding, uncontrolled,” Rabia recalls. “The doctors and nurses were changing the bed sheets after every two or three minutes. They were red with blood.”
She was at a hospital in her hometown of Taxila, north of the Pakistani capital Islamabad. The hospital was small and poorly equipped; it employed hardly any gynaecologists, and did not have the facilities to give Rabia a blood transfusion or to surgically explore the cause of the haemorrhage. As her condition worsened and the bleeding continued unabated, panicked medical staff referred her to a larger hospital, over an hour’s drive away, in the nearby city of Rawalpindi.
By the time she reached the next hospital, everything was a blur. She had lost so much blood that she was experiencing multiple organ failure: her kidneys, liver and lungs were all beginning to fail. In Pakistan, blood banks are generally in short supply, and on top of this Rabia has a rare blood type. In a race against the clock, doctors tested the blood of the relatives who had travelled with her.
Her husband desperately called friends, colleagues, anyone he could think of who could quickly get to the hospital. Those that matched gave blood, which was transfused into Rabia immediately. At the same time, doctors sought to stop the bleeding and warned her family that she might not survive. But, after ten days in hospital, she made a full recovery.
As she struggled to make sense of her experience, Rabia – who five years later is now 31 and studying for a PhD in environmental sciences – looked up every medical paper she could find about the horror she had experienced. As she read, she realised that she was one of the lucky ones. Postpartum haemorrhage is the leading cause of maternal death worldwide, responsible for around 100,000 deaths every year.
The condition is usually defined as blood loss of more than 500 ml within 24 hours of a vaginal birth, or more than 1,000 ml, together with signs of decreased blood circulation, following a caesarean.
While around 6 per cent of women giving birth all over the world – in rich and poor countries alike – develop postpartum haemorrhage, 99 per cent of deaths from it occur in low- and middle-income countries.
Put bluntly, if you develop postpartum haemorrhage in the UK or France, it is extremely unlikely you will die. If you develop it in Pakistan or Nigeria, there is a significant chance that you will. This disparity applies to maternal deaths across the board: 99 per cent of maternal deaths take place in low- and middle-income countries.
Image: Dr Sadia Khan washes her hands before entering the operation theatre at Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
A level of bleeding after giving birth is normal, because a woman has to bleed when the placenta detaches. But for some women, this does not stop. Postpartum haemorrhage can have various causes, but by far the most common is uterine atony. In simple terms: during delivery, the uterus squeezes to push the baby out away from the uterine wall, to which it is attached via the placenta. All being well, the uterus would then contract and seal off the bleeding. Sometimes, that doesn’t happen, so the uterus remains dilated and blood flow is uncontrolled.
In other cases of postpartum haemorrhage, the placenta might not detach entirely. Or the uterus might rupture, causing bleeding inside and out. Or the vagina might be torn, which can cause severe bleeding.
Typical treatment for postpartum haemorrhage involves uterine massage, and drugs such as misoprostol, oxytocin or ergometrine, all of which help the uterus to contract. If this treatment doesn’t work, doctors might take surgical steps – manually removing trapped parts of the placenta, placing temporary sutures on the uterus, stitching external or internal lacerations on the vagina, or, in extreme cases, performing a hysterectomy and removing the uterus altogether.
It can be difficult to identify the cause of the bleeding; during the time this takes a woman may lose a critical amount of blood and, as Rabia did, suffer multiple organ failure. For many, this will cause irreversible damage or death.
It is notoriously difficult to obtain reliable statistics for maternal mortality; a 2015 report by the World Health Organization (WHO) noted that many countries “lack comprehensive systems” for recording these deaths and that “underreporting” is rife.
On the best estimates available, the global maternal mortality rate fell by 44 per cent in the 25 years from 1990 to 2015. While this is a vast improvement, it still means that around the world, more than 200 women die for every 100,000 who give birth.
Image: An operating theatre assistant holds a dose of tranexamic acid before the C-section begins as they are anticipating severe haemorrhaging. Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
In 2009, Haleema Shakur-Still and Ian Roberts, two research scientists at the London School of Hygiene and Tropical Medicine, began to wonder if they might be able to add a tool to the arsenal in the battle against maternal death. They had been working on a clinical trial of a drug called tranexamic acid. The drug, which makes it easier for the body to stem bleeding by stopping blood clots from breaking down, was out of patent and therefore cheap.
It had been invented by husband and wife Shosuke and Utako Okamoto in Japan in 1962. The Okamotos thought it might be a useful treatment for postpartum haemorrhage, but they could not convince local doctors to perform a clinical trial. Instead, tranexamic acid was picked up by a pharmaceutical company and used as a treatment for heavy periods and after tooth extractions.
Shakur-Still and Roberts’s trial, CRASH-2, tested its use on people who were bleeding badly from injuries. The results were striking. If the drug was given intravenously within three hours of injury, it reduced the risk of death by a third. As the two scientists worked with doctors around the world, the subject of postpartum haemorrhage came up again and again.
“Doctors in Nigeria were seeing women come into the emergency department having given birth elsewhere, and bleeding to death,” says Shakur-Still. “It’s so far removed from our experience here [in the UK] that I didn’t even believe that was a reality, until I started looking at the data.”
In March 2010, Shakur-Still and Roberts launched the WOMAN (World Maternal Antifibrinolytic) trial, working in 21 countries to test whether tranexamic acid might similarly reduce deaths from postpartum haemorrhage. The double-blinded trial enrolled 20,000 women with postpartum haemorrhage, randomly assigning them to receive either 1 g of intravenous tranexamic acid, or a matching placebo, in addition to usual care – which would typically consist of uterine massage, one or more of the drugs aimed at helping the uterus contract, or surgery.
Nigeria was the first country to come on board for the WOMAN trial. Around the country, 53 hospitals took part. University College Hospital (UCH) in Ibadan, a sprawling city in southern Nigeria, was the organisational centre.
The thing about postpartum haemorrhage, doctors say, is the chaos. It is a race against the clock to stop the bleeding and find the cause before the patient loses a critical amount of blood and goes into irreversible shock.
Nike Bello, a consultant in gynaecology and obstetrics at UCH Ibadan, has treated too many cases of severe postpartum haemorrhage to count. “[In some cases] we did every single step of surgery, one by one, and she still died. Even after we removed the uterus and ligated all the arteries,” she says. She works at a large, well-equipped government hospital, an expansive complex set back from a traffic-clogged road. The most severe cases end up here, women referred from more basic facilities, often having lost massive amounts of blood before arrival.
Those that stand out in Bello’s mind are the ones that lived. One woman came in having given birth elsewhere, bleeding from lacerations to her vagina. The wounds had been packed with gauze, but it had not stemmed the bleeding. The gauze was soaking red, blood dripping through. “I looked at the vagina and it was all avulsed, it was like someone took a razor to it and shredded it to bits,” says Bello. “I really can’t explain what they did.” Seeing how severe the blood loss was, she decided to take the woman to surgery immediately.
The anaesthetist intervened: there was no blood to replace what she was losing, he said, and what if she died in surgery? In Nigeria, the desperately underfunded healthcare system works on a pay-as-you-go model, where patients and their families must purchase anaesthetic, drugs or blood before medical procedures can be carried out. Payment can be deferred for surgery if a patient cannot afford it, but not for drugs.
The reasoning is that hospitals can absorb the cost of the doctors’ time on surgery but cannot afford to replace medicines that have not first been paid for. If blood banks have stock of the right blood type, patients must buy it before they can receive a transfusion. As there are limited supplies of blood, more often than not, they also have to find a donor. This woman’s family did not have the funds to purchase the blood, and needed to go home to look for more money, which could cause a fatal delay.
“We are saying that if we arrest the bleeding she might die – but if we don’t arrest the bleeding she will die,” Bello told the anaesthetist. “I would rather the patient dies while I am trying to save her than watch her die without trying.”
They took her to surgery. Bello sewed the multiple wounds on the vagina, but the other tissue around it began to tear. As she stitched, the family returned with enough money for four pints of blood. The transfusion was given, and the wounds were eventually sealed off. The woman’s life was saved.
Image: Pharmacist Adebisi arranges some drugs in the pharmacy store as she takes inventory. University College Hospital, Ibadan. Etinosa Yvonne © Wellcome Trust
Nigeria has one of the highest maternal mortality rates in the world; according to the WHO, the country accounts for 19 per cent of all maternal deaths worldwide. Around 800 women die for every 100,000 births. While this figure has lowered over the past two decades, it is still the worst in sub-Saharan Africa. Postpartum haemorrhage is the leading cause. As in other parts of the world, eclampsia – a complication resulting from high blood pressure – is a close second.
Even when a woman survives postpartum haemorrhage, it can have devastating consequences. Oladapo Olayemi, another consultant in obstetrics and gynaecology at UCH, once treated a nurse, an employee at the hospital, who haemorrhaged after giving birth to her first child. The bleeding was severe and nothing was working to make it stop.
As Olayemi operated, he realised he would have to remove her uterus in order to save her life. The woman survived, but for three months afterwards, she would not speak to him, ignoring him when she passed him in the corridor. “Childbearing is a major aspect of our social life,” says Olayemi. “It is seen as a social success to have children, and she only had one. This means you are reluctant to remove the uterus – you have to weigh saving her life. Sometimes you take that decision too late.”
Only 32 per cent of women in Nigeria deliver their babies with a skilled attendant; the vast majority deliver at home, at a basic health facility, or with a traditional midwife. This means that if a woman begins to haemorrhage, there can be long delays before she gets the right treatment. Often, by the time she reaches a large hospital like UCH, she will already have been to two or three smaller hospitals along the way.
This, added to the financial pressure of having to buy medicines and blood before treatment, is a serious logistical problem. Against this context, it is clear why doctors at UCH and elsewhere in Nigeria were eager to take part in the WOMAN trial. But given the scale of the challenges, could tranexamic acid help?
The trial ran for six years, during which time Utako Okamoto, the co-inventor of the drug, died (her husband, Shosuke, had died in 2004). When the results came out in April 2017, they vindicated the Okamotos’ original thesis that it could be effective for postpartum haemorrhage. If tranexamic acid was administered within three hours of birth, the risk of death reduced by 31 per cent, around a third. “It buys us time,” explains Bello. “It makes the bleeding slower, so you can replace blood and fix the problem.”
Before the trial, there were concerns that the drug – which encourages blood clotting – might have an adverse effect since pregnant and lactating women are already prone to blood clots. But the trial showed that it did not. “For us in Nigeria, [the results] are very significant,” says Bukola Fawole, a professor at UCH and Nigeria’s project lead on the WOMAN trial. “If postpartum haemorrhage accounts for 25 per cent of all maternal deaths, and if we utilise tranexamic acid in every woman who is bleeding sufficiently early, it will reduce almost a third of those deaths. For us, that is huge.”
The WHO updated its recommendation on using tranexamic acid for postpartum haemorrhage in light of the WOMAN trial. But almost two years after the results came out, the drug isn’t always easily available in the countries that need it most. Tranexamic acid is cheap, heat-resistant, easy to store and to produce, and it is proven to save lives. Why aren’t we using it everywhere?
In 2010, Rizwana Chaudhri, the dean of Rawalpindi Medical University in Pakistan, attended a conference for obstetricians and gynaecologists in London. She picked up a leaflet that asked: “Would you like to be part of a trial to save mothers?” As she sat in the conference hall, she got out her phone and emailed right away. “Postpartum haemorrhage is one of the main killers in our country,” she tells me. “Anything we can do to save even one human life, with any added drug, would be beneficial.” She soon became the WOMAN project lead for Pakistan.
The Holy Family Hospital in Rawalpindi, where Chaudhri practises, was the centre of the trial. Twinned with the capital Islamabad, Rawalpindi is Pakistan’s fourth-largest city, a densely populated maze of streets. Pakistan’s population is rapidly growing: this hospital alone delivers 21,000 babies annually, Chaudhri says. Demand far outstrips the facilities.
Image: Patients and their relatives at the high-risk postnatal ward at Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
On the postnatal ward, beds are shared by two women, sometimes three, and their babies. In the nursery, where premature babies and those with jaundice or other serious problems are cared for, incubators designed for one baby are filled with five or six, lined up next to each other with name tags around their wrists.
This is a government hospital, so patients receive free medical care, and no one is turned away. It serves a huge geographical area encompassing both urban centres and far-flung villages. Like UCH in Ibadan, it is a referral centre, and by the time women reach this hospital after giving birth at home or in a basic health unit, they may have already lost a critical amount of blood.
“Death usually occurs when there is a delay,” explains Chaudhri. “The golden period is the first three hours. There are three main delays. The first is decision making. The woman is not empowered enough to decide, ‘I’m going [to the hospital].’ The family decides and they may have to contact their males. The second is money – they may not have transport. The third is the distance they have to cover, and that they have no idea where to take them, so they go from one facility to another.”
According to Sadia Khan, a consultant in obstetrics and gynaecology, the Holy Family Hospital typically sees two women a day with severe postpartum haemorrhage. The role of poverty and the marginalisation of women is hard to ignore.
“In Pakistan, the fertility rate is high and the inter-pregnancy interval is low – a woman might be having a baby every year, which is a risk factor,” says Khan. “Especially in rural areas, the mother is probably the last person in the household who is the priority.”
Poor nutrition means that more than 50 per cent of Pakistani women of reproductive age are anaemic, compounding the problem of postpartum haemorrhage: if a mother’s haemoglobin levels are already low, she is less able to withstand heavy blood loss. The vast majority of women do not seek any antenatal care at all, meaning they might be unaware that they are anaemic and therefore at high risk of complications.
In the most extreme cases of haemorrhage, women enter a state called disseminated intravascular coagulation, when all the blood in their body fails to coagulate. This can cause bleeding from elsewhere – the gums, the nose. At this stage, it is very hard to save their life.
Image: A mother with her newborn baby at the high dependency unit a few hours after her delivery. Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
In 2016, two years after her stillbirth, Rabia was pregnant again. She had read everything she could find online about postpartum haemorrhage, and spoke to her family doctor in Taxila to ask what could be done to prevent a recurrence. The doctor told her about the trial for tranexamic acid. Rabia left the appointment and scoured the internet for information about the trial.
“I found the whole literature, the WOMAN project, this trial going on globally,” she says. As the due date approached, she anxiously prepared. Her husband gathered blood donors from among their friends and family, and this time they went straight to a large hospital when she went into labour.
After giving birth to a healthy baby girl, the bleeding started again. The horror of her last experience, the uncontrolled bleeding and the organ failure, rushed back to Rabia. “I was thinking that history is going to repeat,” she says. An injection of tranexamic acid was delivered, alongside other measures such as intrauterine packing with gauze and manual removal of placenta pieces that had failed to detach. Miraculously, it seemed to Rabia, the bleeding stopped. Within a day, she had made a full recovery. The tranexamic acid “made a difference, definitely,” she says.
When the trial results came out in April 2017, the doctors who had worked on it in Pakistan were jubilant. Tranexamic acid, which stops blood clots from breaking down, works in a totally different way from other drug treatments for postpartum haemorrhage, which mainly focus on helping the uterus to contract. “If the patient has had the uterotonic drugs and needs two transfusions, the addition of tranexamic acid means the need for blood transfusions is reduced, as is the need for surgery,” explains Khan. “It’s easily available, cheap, very effective. It’s a magic drug.”
Zainab lives in Ibadan, Nigeria. When she went into labour seven years ago, she decided to go to UCH, where she worked as a health attendant. She felt perfectly well, but it was her first child, so she didn’t know what to expect and didn’t want to take any risks. Her husband was at work, but she didn’t ask him to go with her. She walked into the hospital herself and presented at the labour ward.
At first, things went smoothly. Her child was delivered, a healthy baby boy. After that point, her memory is hazy.
“I can’t even explain, the music changed within two seconds. I knew I had a baby boy, but the only thing I can remember is opening my eyes and seeing I was in an anti-shock gown.” These compression garments are sometimes used to stem bleeding.
Zainab remembers a doctor explaining to her that a trial was going on, and that there was an injection that might stop the bleeding. She agreed to have it. She was absolutely sure that she was going to die. The doctors administered tranexamic acid along with a blood transfusion. She doesn’t know how long it took, but the bleeding stopped.
“I thank god that research was going on there,” she says. “In short, I am alive. My baby is doing fine. Without that research, I might not be alive today.”
Although she was careful about her health and sought medical support during her pregnancy, Zainab had never heard of postpartum haemorrhage.
“I knew women were dying in delivery, I knew things happened, but I thought I could never be a victim.” In May, her son will be seven. She often thinks about the trial. “If this drug was not available, where would I be today? Who would be taking care of that poor boy?”
Image: Dr Sadia Khan, with her team of doctors and technicians, preparing for a C-section on a woman who is at risk of postpartum haemorrhaging. They have arranged for tranexamic acid and blood for transfusion to be ready in the operation theatre. Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
In fact, now that the trial is over, tranexamic acid is not available in much of Nigeria, or in many other countries where maternal mortality is high. Nigeria’s health minister Isaac Adewole, a gynaecologist by training, issued a directive recommending that every hospital in the country stock it. But progress has been slow, in the face of underfunding and poor infrastructure.
“The drug is available, but not as widely available as we would wish,” says Bukola Fawole, the country’s WOMAN project lead. “We want it to be available in every nook and cranny.” He and his colleagues have been running sessions with gynaecologists, obstetricians and midwives to raise awareness of the drug. These efforts are ongoing, but the problem of distribution remains. Tranexamic acid is not produced in Nigeria.
The price increased after the trial results – perhaps because of increased demand, as well as a simultaneous collapse in the Nigerian currency. During the trial, the drug was provided for free to the 50 hospitals that took part. Today, even those hospitals do not all stock tranexamic acid, because of the cost and the difficulty of finding a reliable supplier.
According to Tolulope Adebisi, the pharmacist at UCH in Ibadan, it can be challenging to get hold of tranexamic acid. Hospital pharmacies work privately, on a supply-and-demand basis. If a doctor doesn’t prescribe a drug, pharmacists won’t stock it, but this can become a vicious circle, as doctors won’t prescribe drugs that are not routinely stocked.
“Drug companies don’t want to tie up their capital with drugs like that, except if they are sure of a ready market,” says Adebisi. “They prefer antibiotics, antimalarials, things that are fast-moving.”
At a large teaching hospital such as UCH, pharmacists have well-developed relationships with a range of suppliers, and are more easily able to stock tranexamic acid.
“We have our regular reliable suppliers,” she says. “For smaller hospitals, it might be more difficult to access.” A vial of 500 mg of tranexamic acid can cost 1,500 naira (£3.20), and two would be needed for the recommended dose. This is significantly more expensive than the other drug treatments for postpartum haemorrhage – a further deterrent for patients. According to Adebise, some cheaper versions of the drug are becoming available, but they are still not widely accessible.
This is all the more frustrating, because where tranexamic acid is being used, it appears to be having an effect.
“We still encounter postpartum haemorrhage a lot, it is still very common, but they don’t die,” says Oladapo Olayemi, one of the consultants at UCH. “Locally here, the hospital has adopted it, and the impact was immediate.” He notes a general improvement in maternal outcomes alongside the impact of tranexamic acid – with traditional midwives, for instance, being faster to refer women to hospital when they are experiencing haemorrhage.
Maternal mortality remains high in certain countries for a complex host of reasons going far beyond the actual medical complications – from poor nutrition to the marginalisation of women.
In much the same way, the challenges in implementing new treatments are multifaceted. Studies suggest that there is typically a time lag of 17 years between a successful clinical trial result and a drug being widely in use around the world. The reasons for this can vary. It takes time to change human behaviour, and for doctors to integrate a new treatment into their arsenal. Drug supply can also be an issue. And in countries such as Pakistan and Nigeria, where state infrastructure is weak, implementation of recommendations can be slow.
In some countries that took part in the trial, such as Uganda, tranexamic acid is barely being used.
“The infrastructure is just not there in some places,” says Ian Roberts, one of the trial directors at the London School of Hygiene and Tropical Medicine.
This problem is not unique to tranexamic acid. Creating a market for a new drug, or for a new use of an old drug, is a laborious and unglamorous process. In international development parlance, this is referred to as “market shaping”, attempting to create a balance where there is enough demand for a drug to make it profitable for pharmaceutical companies but also good value for the countries purchasing it.
Many doctors have been unaware of what tranexamic acid can do. In Pakistan, faced with so many cases of postpartum haemorrhage and too little use of the drug to treat it, Rizwana Chaudhri decided to take action.
“What is the use, putting in so much effort and money, and it goes on the shelves?” she says. The country has a well-developed pharmaceutical industry, and unlike in Nigeria, several companies produce tranexamic acid domestically, meaning that it is cheap and easily available.
Soon after the trial results, Chaudhri got in contact with one of the largest of these, Hilton Pharmaceutical. In the absence of public funding to disseminate news of the successful results, the company funded Chaudhri and her colleagues to hold seminars around the country to inform clinicians about the new use for tranexamic acid. So far, sessions have been held in Pakistan’s major cities – Islamabad, Karachi, Lahore, Peshawar and Quetta – with plans for more over the next year.
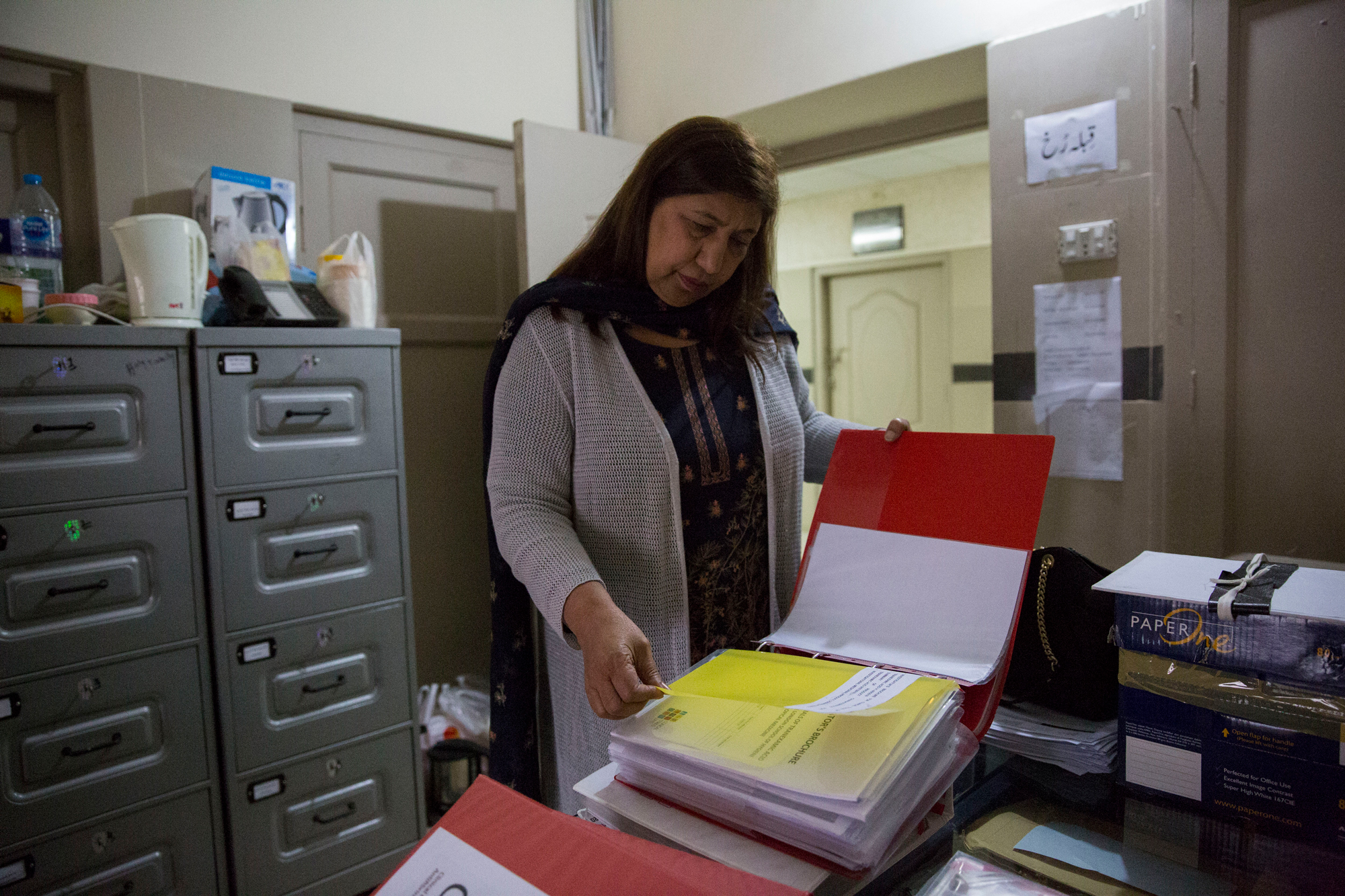
Image: Dr Rizwana Chaudhri goes through the study file for the WOMAN trial at the department of obstetrics and gynaecology at Holy Family Hospital, Rawalpindi. Saiyna Bashir © Wellcome Trust
Given its easy availability in the country, the drug was already widely used for a variety of conditions, but if it was used for postpartum haemorrhage, this was ad hoc given the lack of clinical evidence.
“Previously, even if it was practice to give tranexamic acid, it was usually given late – if you tried everything else and that failed,” says Chaudhri. “But this trial has proved that this is first-line management. Everybody who has the knowledge is now using it.”
When it comes to reducing maternal mortality, there are many contributing factors that have nothing to do with the drugs on offer. In both Pakistan and Nigeria, as well as in a host of other lower-income countries, women in rural areas may not have easy access to a proper hospital in which to deliver; if they are referred, there are often no ambulance services to transfer them.
Even if gynaecologists and obstetricians at hospitals know what to do and how to do it, staff at more basic healthcare facilities will still be ill-equipped to treat postpartum haemorrhage.
“We need to train people,” says Chaudhri. “Even if they’re not well-versed with all the procedures, they should know how to transfer the patient, do the packing and give an IV line.”
The next stage of the WOMAN trial will explore whether tranexamic acid can prevent postpartum haemorrhage when it is given to high-risk women, such as those with anaemia, before any haemorrhaging has started.
“For lots of women, by the time they start bleeding, it’s almost too late,” says Haleema Shakur-Still, one of the trial directors. “We wondered if we give tranexamic acid even before they start to bleed, whether you can prevent postpartum haemorrhage happening in the first place.” The researchers are also exploring alternatives to intravenous use, such as a drinkable dose or intramuscular injection.
This would make treatment much easier at basic health units, where staff may not have the expertise to administer a drug intravenously.
In late 2018, Rabia gave birth for a third time, to her second healthy child. Having experienced postpartum haemorrhage twice, she made the decision, with her doctor’s advice, to have a caesarean. An injection of tranexamic acid was administered. There were no complications. “My experiences were horrible and when I recall that time, it is terrifying,” she says. “To conceive is a great thing. But the matter of concern is to have a safe pregnancy, a healthy baby and healthy mother.”
Since his interview for this piece, Professor Bukola Fawole has died.
Wellcome, the publisher of Mosaic, co-funded the first WOMAN trial and is supporting the next stage.