Continuing pneumococcal conjugate vaccine in Kenya at full price is cost-effective and could save thousands of children’s lives
16 April 2019 London School of Hygiene & Tropical Medicine London School of Hygiene & Tropical Medicine https://lshtm.ac.uk/themes/custom/lshtm/images/lshtm-logo-black.png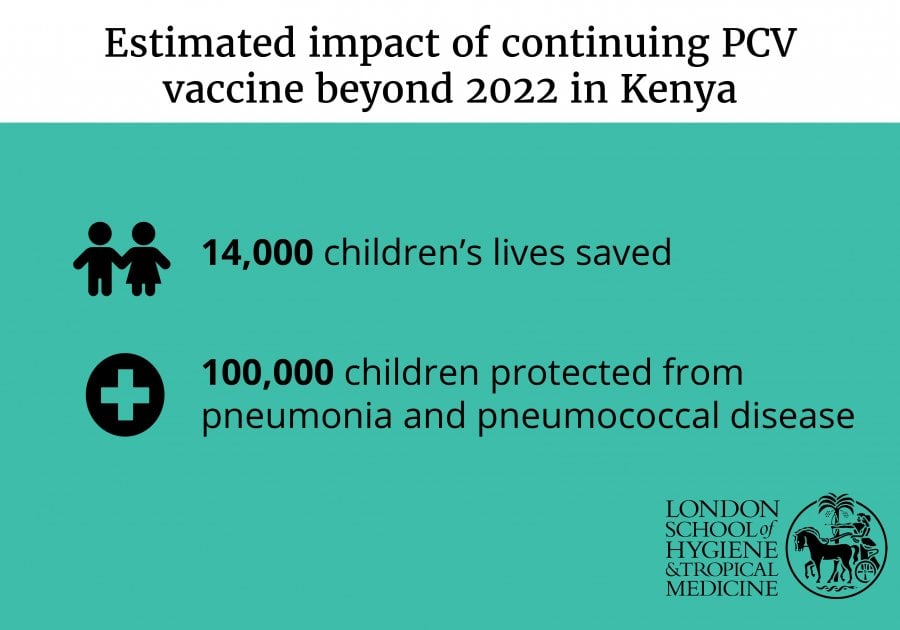
Continuing the pneumococcal conjugate vaccine (PCV) in Kenya after the country transitions away from Gavi, the Vaccine Alliance, support is highly cost-effective and estimated to save thousands of children’s lives, according to new research published in The Lancet Global Health.
Co-led by the London School of Hygiene & Tropical Medicine and the KEMRI-Wellcome Trust Research Programme, the Pneumococcal Conjugate Vaccine Impact Study estimated that continuing the vaccine beyond 2022 would prevent – in the first ten years – more than 100,000 children and adults from contracting pneumococcal disease and save the lives of 14,000 children and adults who would otherwise have died.
The cost per year of healthy life saved (US $153) was considerably less than Kenya’s annual gross domestic product (GDP) per person (US $1,790 in 2018), which meets – and far exceeds – the World Health Organization (WHO) GDP-related threshold for ‘very cost-effective’ health interventions.
The researchers say this study offers important evidence for policymakers at what is a crucial time for countries that have to decide whether to continue vaccine programmes that have benefited from Gavi’s subsidy of the cost of vaccines once their economies grow and Gavi support diminishes.
Lead author Dr. John Ojal, of the London School of Hygiene & Tropical Medicine and the KEMRI-Wellcome Trust Research Programme, said: “If the Kenyan government decides not to continue the vaccine beyond January 2022, and children born after this time are no longer vaccinated with PCV, the incidence of invasive pneumococcal disease will rebound to that experienced before the vaccine was introduced. This is because there will be a growing pool of children who are not directly protected by vaccination and also not indirectly protected by vaccination of individuals around them.”
PCV was introduced in Kenya in 2011 in order to protect children from pneumonia – one of the leading causes of death in children under five. Recent research has shown that PCV has reduced hospital admissions due to pneumonia by over a quarter.
At present, Kenya contributes just US $0.21 to the full cost of the vaccine, thanks to support from Gavi. By 2022, Kenya will enter an ‘accelerated transition’ phase, which will see the Gavi subsidy reduce rapidly until 2027, at which point Kenya will pay the full Gavi-negotiated price the country is eligible for. At US $3.05 per dose, this is a fraction of the per-dose cost of US $180 in the USA, but 15 times more than what Kenya is paying now.
To estimate the cost-effectiveness of continuing PCV after 2022, researchers combined data from ongoing detailed health surveillance in Kilifi, Kenya with mathematical modelling and health economics in order to determine the cost-effectiveness of continuing the pneumococcal conjugate vaccine programme beyond 2022.
Anthony Scott, Professor of Vaccine Studies at the London School of Hygiene & Tropical Medicine and Principal Investigator of the Pneumococcal Conjugate Vaccine Impact Study said: “Many low-income countries that receive Gavi support – including Kenya – will soon have to make vital decisions about whether to continue PCV use at full costs as they transition away from Gavi support. Studies like these are crucial so that policy makers can make evidence-based decisions that will impact on the health of their populations.”
Researchers estimated that continuing PCV beyond 2022 will cost Kenya US $15.8 million per year – more than double the current total vaccine budget. After transition away from Gavi support, Kenya’s financial contribution to other Gavi-supported childhood vaccines, such the pentavalent vaccine and those for yellow fever and rotavirus, will also have to increase.
John Ojal said: “This puts further stress on Kenya’s health budget, so while our findings support an expansion of the vaccine budget, affordability may be a concern.”
Work is ongoing to reduce the cost and improve the cost-effectiveness of the PCV programme: development of a cheaper vaccine, trials to reduce the number of required doses, and research by the KEMRI Wellcome Trust Research Programme and London School of Hygiene & Tropical Medicine to assess the effectiveness of smaller vaccine doses.
The authors acknowledge the limitations of the study, including that no local information was available about the proportion of children among non-hospitalised pneumonia patients who were treated as outpatients, and that the cost-effectiveness analysis is largely based on the assumption that reduction in disease will translate to reduction in mortality.
The study was funded by the Wellcome Trust and Gavi, the Vaccine Alliance.
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.
