a-close-up-of-a-bacteria
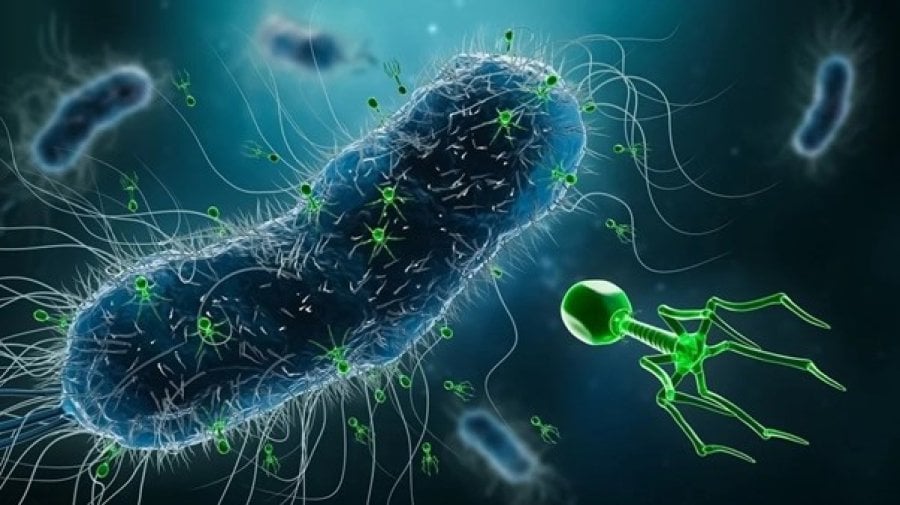
AMR is increasing worldwide, and our antibiotic arsenal is becoming more susceptible to bacteria it once eliminated. A potential tool against this threat is bacteriophage (or phage) therapy. Phages are a group of viruses that infect and kill specific bacteria. Thus, phage therapy refers to the use of phages to treat infections.
Phage Therapy History and Applications
Phage therapy has been used for over 100 years, but its application remains experimental. With the quick and promising success of antibiotics, and its subsequent massive production in the 1940s, phage therapy was placed on the back burner. There have been several attempts to reinvigorate phage therapy use; for example, in 2007, the FDA and Canadian Environmental Protection Agency approved 2 anti-listeria phage solutions for food products– one of the first reintroductions of phage therapy cocktails in these countries [1].
Phages are currently used in experimental, often life-threatening cases where antibiotics have failed in patients, and have had encouraging results. The first use of phage therapy in the USA was in 2016, to successfully treat a severe multidrug-resistant (MDR) Acinetobacter baumannii infection. This particular case gained worldwide attention and has led to an increase in phage therapy research since.
Phages are highly specific to bacterial hosts and are not pathogenic to human cells, offering advantages over the indiscriminate nature of antibiotics that can kill useful bacteria. Phages can also dismantle biofilms that bacteria can develop – often contributing to resistance - making bacteria sensitive to antibiotics once again [2]. Therefore, phages have the exciting potential to be used in conjunction with antibiotics or by themselves.
Challenges
Nevertheless, there are several challenges in perfecting phage therapy against AMR. Firstly, the high specificity of phages makes it difficult to identify and isolate optimal phages for target pathogens. This also makes it difficult to stabilise phages as they constantly evolve in their environment. As with antibiotic resistance, bacteria can also evolve phage resistance. Phages have been very responsive to bacterial resistance so far, but we cannot rule out this threat.
In response to these challenges, tools such as genomic sequencing and artificial intelligence (AI) may be used to better identify and stabilise phages. Eventually, scientists hope that we may also be able to optimise specific phages according to diseases and individualised human microbiota.
In the UK, phage therapy research and development are at an impasse due to lack of funding and regulatory limitations. There have been no clinical trials since 2009 [3]. It is vital that regulatory bodies consider the expansion of phage therapy in the medical sphere, allowing more clinical trials to take place. However, development is taking shape in many research centres such as the University of Leicester, where its Centre for Phage Research plans to create a phage biobank [4].
Phage therapy is an exciting and promising tool against the growing threat of AMR. As we reinvigorate research into this therapy, there are many possibilities to use phage therapy with and without antibiotics.
References
Brives C, Pourraz J. Phage therapy as a potential solution in the fight against AMR: obstacles and possible futures. Palgrave Communications [Internet]. 2020 May 19 [cited 2024 Apr 14];6(1):1–11. Available from: https://www.nature.com/articles/s41599-020-0478-4
Science, Innovation and Technology Committee. The antimicrobial potential of bacteriophages [Internet]. UK Parliament. UK Parliament; 2024 Jan [cited 2024 Apr 14]. Available from: https://publications.parliament.uk/pa/cm5804/cmselect/cmsctech/328/repo…;
Science and Technology Committee. Oral evidence: The Antimicrobial Potential of Bacteriophages, HC 886 [Internet]. UK Parliament. UK Parliament; 2023 [cited 2024 Apr 14]. Available from: https://committees.parliament.uk/oralevidence/12669/pdf/
University launches pioneering new centre to study bacteriophages to combat antibiotic resistant bacteria | News [Internet]. University of Leicester. 2023 [cited 2024 Apr 14]. Available from: https://le.ac.uk/news/2023/may/martha-clokie
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.
