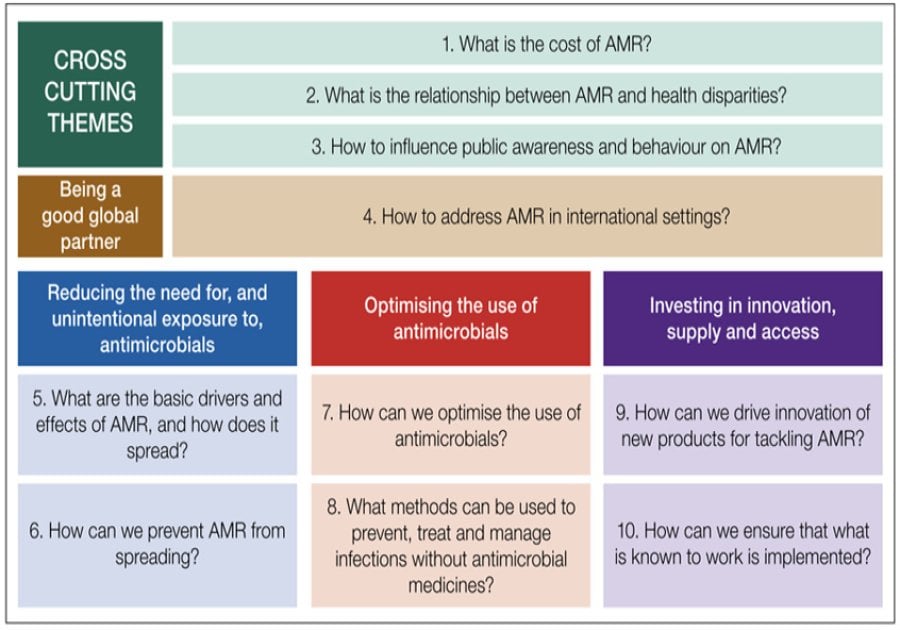
Figure from the recent UK National Action Plan on AMR 2024-2029 showing the exciting 10 research priorities
The UK is a global leader in the collation and analysis of AMR data, in the formation of National Action Plans (NAPs) and in engaging communities in AMR control. The most recent iteration of the UK NAP was launched in mid-May 2024 and lays out ambitious plans for tackling both the UK and global problem. The NAP has the underlying principles of taking a collaborative approach across the UK, maintaining a One Health response, being a good global partner to reduce inequalities and maintain resilience across four themes with nine strategic outcomes and thirty commitments. Overall, it is an exciting document for the AMR community in its ambition and reach. Key to this ambition are the human health targets (though specific targets for data linkage are absent) and the detail given to research priorities (Figure 6, shown above).
Introduction
The report starts with an overview of the threat of AMR, reflecting on the UK response both going forward in the wake of COVID-19 and in terms of how far progress has been made since the previous 5-year NAP. Substantial achievements are noted, especially in reducing the use of antibiotics in food-producing animals (59%). However, the analysis by the LSHTM National Institute for Health and Care Research (NIHR) Policy Innovation and Evaluation Research Unit (PIRU) team (as yet unpublished) pointed to areas where progress could be made. Data linkage needs to be improved and implementation lessons could be learned from other settings where different policy directions have been taken. Linked to the recent focus on pathogen spread in water, the UK water industry is noted as having an opportunity to play a meaningful role in addressing AMR.
The stated underlying principles reflect how thoughtfully this NAP has been developed (see Appendix A for more information on the consultative process) and the focus on tackling health disparities and health inequalities is very welcome. Moreover, it makes a lot of sense to talk to resilience in the face of changing pandemic threats and climate change. It would have been good in the burden analysis to emphasise or at least include the wide uncertainty on all the values quoted (from IHME analysis) especially as it is emphasised throughout that data linkage and burden estimates need further investment.
Theme 1: Reduce the need for and unintentional exposure to, antimicrobials
The first theme tackles infection prevention and control, public awareness of antimicrobial exposure and strengthened surveillance, with two human-health infection targets for 2029: to prevent increases in a set of drug-resistant infections, and all Gram-negative bloodstream infections, from a 2019 level. The list of DRIs is in table 2.3 of the ESPAUR report annexe and includes MRSA, carbapenem resistant E. coli and K. pneumoniae. This theme also has a target to increase UK public and healthcare professional’s knowledge on AMR by 10% with a commitment to increase use of educational settings. It would be great to see more on AMR in the UK national curriculum. The third outcome on strengthened surveillance is lacking in targets for data linkage with lots of “aims to measure” and “optimise” when ambitious data linkage targets could have been put in place e.g. to build a linked primary and secondary care database of antibiotic usage covering x% of patients? Or to build a resilient system that records IPC interventions individual hospitals are putting in place and hence could be used to explore intervention efficacy building on our experience with COVID-19? The Zambia One Health surveillance platform, based on discussions with Zambian colleagues, is also still in early stages and may have been over-emphasised in terms of its current utility. Overall, though, this theme lays out important commitments to stop infections and hence prevent rather than firefight AMR.
Theme 2: Optimising use
The second theme tackles antimicrobial stewardship and the AMR workforce with headline human health 2029 targets to reduce total antibiotic use in human populations by 5% from the 2019 baseline and 70% of total use to be from Access antibiotics. This is vital to protecting our Watch and Reserve antibiotics, especially in the UK where most antibiotics are now consumed by humans and “human use drives AMR in bacteria in humans”. Here it was great to see the emphasis on a shift to “whether to prescribe” instead of “what to prescribe”, with a focus on clinical decision support and risk stratification tools potentially using powerful artificial intelligence (AI) algorithms. Building on the comments above – this will only be possible if the data can be effectively linked and shared, and properly understood by improved collection of bias and sampling frameworks to ensure nuance in denominators. This theme emphasises the importance of behavioural interventions to support, for example, the shift to shorter treatments (where further studies are called for) and links to Theme 1 with a focus on system-wide infection management and governance. Importantly, whilst the commitments to support veterinarians are separate, they are clearly embedded in wider systems thinking and build on the great progress that has been made in One Health monitoring, antibiotic reductions and clear targets in several food production systems in the UK.
Theme 3: Investing in innovation, supply and access
The third theme is about investments, with a focus on developing a suite of new tools, technologies and interventions, including the subscription model for new antibiotics. An interesting statistic quoted here is that the UK represents only 3% of the global antimicrobial market and hence must work with the wider global pipeline to drive new antimicrobial discovery. Mentioned here are the learnings from COVID-19 and the clinical trial infrastructure that could be harnessed for new AMR tools, but with the careful caveat that new antimicrobials must go hand in hand with antimicrobial stewardship and an understanding of the social science of adoption.
The most exciting part of this theme for the wider academic community is outcome 7: using “information for action” with clarity around 10 research priorities (shown in the figure above). The phrasing of these questions and the focus they put on both understanding the epidemiology of AMR (drivers/spread) as well as the actions to tackle AMR is aspirational for the wider AMR research field. The importance placed on these questions, and the thought given to them, is emphasised in the detailed example sub-questions in Appendix C.
The rest of this theme is also highly important and needed: a whole outcome focused on untangling the link between AMR and heterogeneity in health disparities and inequalities will be vital to improve our understanding of AMR through better-linked data to support improved nuance and impactful interventions.
Theme 4: being a good global partner
The final theme recognises that the UK does not stand alone against AMR, with the commitment to being a good global partner through being a “best practice” example in the UK and engagement with global groups. This builds on an established practice of doing this in the UK for example through the Fleming Fund which comes over as a key part of the first commitment on prevention and preparedness. The four other commitments (on access and stewardship, antimicrobial use in farming, manufacturing and waste management standards, advocacy and engagement) follow the pattern of developing strategies and standards in the UK to the advocate for use globally.
Personal reflection
I would agree that the “ambitious course of action” does indeed strengthen the UK commitment to prevent infections, optimise antimicrobial use and invest in research and innovation. I would have liked to see a clearer target to improve linkage of data on antibiotic use, microbiology, resistance and clinical outcomes across primary and secondary care and the wider environment. However, as this is so fundamental to answering the detailed research questions I am hopeful that a lot will be achieved by 2029 in the UK, especially in untangling the link between AMR and health inequalities.
Reference
Confronting antimicrobial resistance 2024 to 2029 (08/05/2024), https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobial-resistance-2024-to-2029/confronting-antimicrobial-resistance-2024-to-2029#appendix-b-human-health-targets%22%20%EF%B7%9FHYPERLINK%20%22https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobial-resistance-2024-to-2029
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.
