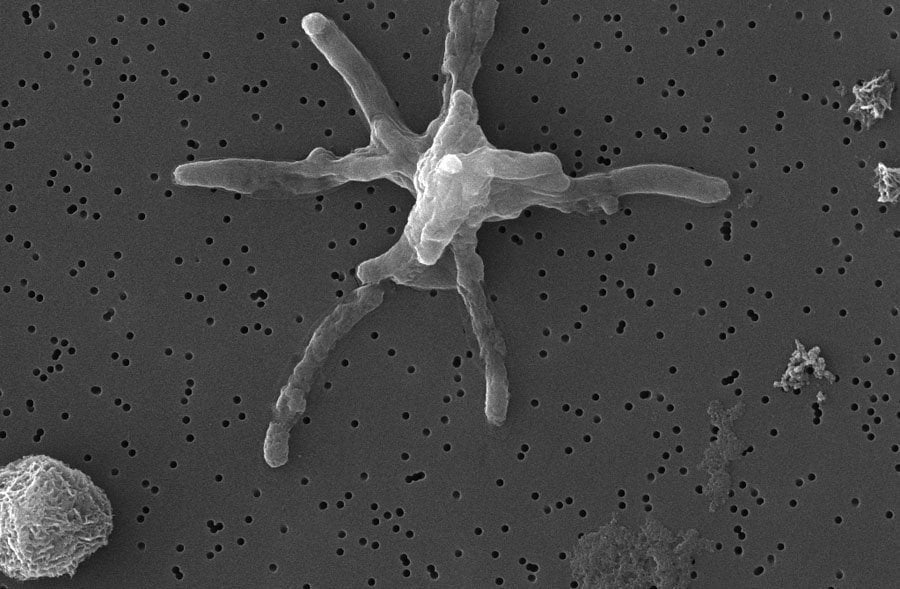
M. tuberculosis micrograph courtesy of Dr Clara Aguilar Pérez
Tuberculosis (TB) is an infectious disease caused by the bacterium Mycobacterium tuberculosis. Despite being treatable, TB remains one of the leading causes of death worldwide, particularly in low- and middle-income countries. The emergence of drug-resistant strains has compounded the difficulty in controlling the disease, highlighting the urgent need for new and effective treatments. In this week’s spotlight, Richard Wall, an AMR centre committee member, shares a brief history of TB drug discovery and the challenges of developing new drugs to eradicate TB.
A very concise history of TB drug development and treatment
The pursuit to discover effective treatments for TB has a rich history marked by significant milestones in drug discovery and development. The first major breakthrough came in the 1940s with the discovery of streptomycin, the first antibiotic effective against TB. This was followed by the introduction of para-aminosalicylic acid (PAS) and isoniazid, which together formed the basis of the first standard combination therapy for TB in the 1950s. The 1960s saw the addition of rifampicin and pyrazinamide, which revolutionised TB treatment by shortening the duration of therapy. This combination therapy approach, known as DOTS (Directly Observed Treatment, Short-course), became the standard for TB control worldwide and is largely considered one of the most significant health breakthroughs of the time. However, the emergence of drug-resistant TB in recent decades has posed significant challenges, necessitating ongoing drug discovery efforts. After a long delay in the discovery of new antitubercular drugs, recent advances in TB drug discovery resulted in new drugs such as bedaquiline and delamanid. However, given the continuous evolution of M. tuberculosis, there is a critical need for continuous innovative research and drug development to treat drug-resistant TB infections.
The rise of drug resistant-TB
Rifampicin quickly became a cornerstone of TB treatment due to its potent bactericidal activity. However, resistance to rifampicin soon emerged, often as a result of improper use, such as incomplete or inconsistent treatment. Rifampicin-Resistant TB (RR-TB), characterised by resistance to rifampicin alone, was recently included in 2024 WHO bacterial priority pathogen list (BPPL), highlighting the significant impact that the loss of rifampicin, as a treatment option, poses for treatment outcomes. Multidrug resistant-TB (MDR-TB) is defined as TB that is resistant to rifampicin and at least isoniazid, the two most powerful antitubercular drugs in first-line (drug sensitive) treatment. The prevalence of MDR-TB began to rise in the 1980s and 1990s, driven by factors including inadequate TB control programmes, patient non-adherence to treatment regimens, and the lack of new drugs. Treating MDR-TB is challenging, often involving lengthy, toxic, and expensive regimens with second-line drugs. In 2022, RR-TB and MDR-TB accounted for approximately 160,000 deaths related to TB. Finally, extensively drug resistant-TB (XDR-TB), a more severe form of MDR-TB, is resistant not only to rifampicin and isoniazid but also to any fluoroquinolone and at least one of the three injectable second-line drugs (amikacin, kanamycin or capreomycin). First identified in the early 2000s, XDR-TB poses a particularly serious threat due to the limited treatment options available and higher mortality rates. Today, there are already reported cases of bedaquiline resistance, considered a key drug in the fight against drug resistant-TB, highlighting the critical importance of continued research into novel therapeutic agents to address and mitigate the impact of TB globally.
The challenges of TB drug discovery
One of the primary challenges in TB drug discovery is the complex biology of M. tuberculosis. The bacterium’s thick, waxy cell wall, composed of mycolic acids, makes it inherently resistant to many potential drugs, complicating drug penetration and effectiveness. Exacerbating this is the dearth in validate drug targets, limited tools to identify the targets of new phenotypically active compounds from screening programmes and appropriate animal models to show efficacy in vivo. Additionally, the slow growth makes laboratory studies and drug efficacy tests time-consuming. M. tuberculosis can also enter a dormant state within the host, becoming metabolically inactive and highly resistant to most drugs, complicating eradication and leading to disease relapse even after prolonged treatment. As highlighted above, the emergence of MDR-TB and XDR-TB further exacerbates the challenge, necessitating new drugs and complex, toxic treatment regimens. In the clinic, there are also many economic and regulatory barriers, as well as public health challenges, such as the undue stigma surrounding infected TB patients.
Current state of the antitubercular drug pipeline
The World Health Organisation (WHO) recently released its latest report on antibacterial agents in clinical and preclinical development worldwide. This showed a >20% increase in the number of antibacterial agents in the clinical pipeline, although it emphasised a pressing need for a significant increase in innovative treatments for serious infections. The list included 19 new “direct acting small molecules” in development against TB and drug-resistant TB although only 8 were considered innovative (specifically a novel mode of action). Two compounds in particular have advanced to phase II/III clinical development. SQ109 targets the mycolic acid transporter (MmpL3), a critical component for bacterial cell wall synthesis. It successfully completed a Phase IIb/III clinical trials in Russia, highlighting its efficacy in diverse populations. Sudapyridine (WX-081) is a novel diarylpyridine, based on an optimised version of bedaquiline, but with improved pharmacokinetic and safety profiles. This optimisation is expected to lead to better patient outcomes and reduced side effects. Currently, patients are being enrolled in a Phase III clinical trial in China, which aims to confirm its efficacy and safety on a larger scale, potentially making it a significant addition to the TB treatment arsenal. Both SQ109 and Sudapyridine represent promising developments in the fight against TB, addressing the need for more effective and safer treatment options, especially in the face of increasing drug resistance.
In conclusion, TB remains a formidable global health challenge due to its complex biology and the persistent threat of drug resistance. Indeed, it is thought to affect up to two billion people globally and resulted in 1.3 million deaths in 2022 alone. While significant strides have been made in TB drug discovery and treatment, continued innovation and collaboration are essential. Addressing TB effectively requires sustained investment in research and development of new therapies with novel modes of action.
References
Iseman, M. D. (2002) Tuberculosis therapy: past, present and future. European Respiratory Journal 20, 87-94.
Murray, J. F., Schraufnagel, D. E. & Hopewell, P. C. (2015) Treatment of Tuberculosis. A Historical Perspective. Ann Am Thorac Soc 12, 1749-1759.
TB alliance (2023) Why new TB drugs?
World Health Organisation (2024) WHO bacterial priority pathogens list, 2024: Bacterial pathogens of public health importance to guide research, development and strategies to prevent and control antimicrobial resistance.
World Health Organisation (2024) 2023: Antibacterial agents in clinical and preclinical development: an overview and analysis.
World Health Organisation (2023) Global Tuberculosis Report 2023.
World Health Organisation (2023) New treatment for drug-resistant tuberculosis.
Yao, R. et al. (2022) Sudapyridine (WX-081), a Novel Compound against Mycobacterium tuberculosis. Microbiol Spectr 10, e0247721.
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.
