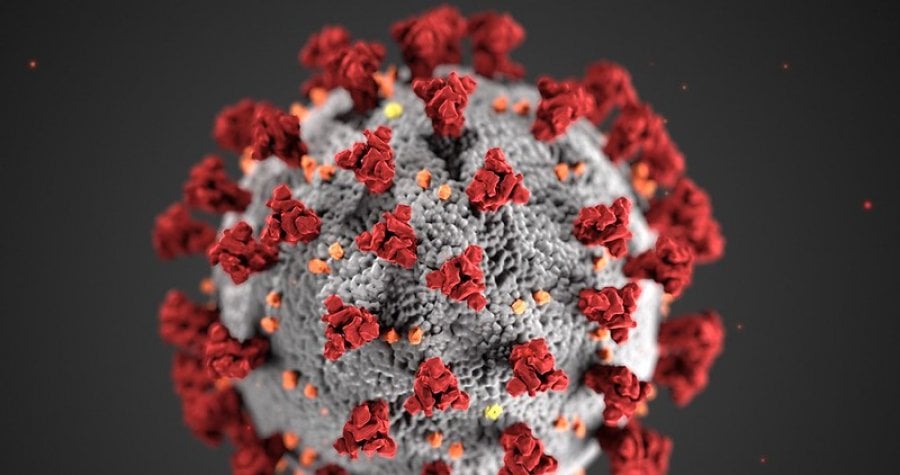
COVID-19
Read the complete paper here.
On Friday 27 March, President Emmerson Mnangagwa of Zimbabwe declared COVID-19 a national disaster. In the following days, the government enacted a nationwide lockdown, launched a media campaign, and barred all non-essential travel. Facing an under-resourced public health system, the Ministry of Health mandated a stringent response to curb the spread of COVID-19. As of Monday 27 April, there were 31 confirmed cases and four deaths in Zimbabwe and over 30,000 cases across Africa.
But are Zimbabwean government guidelines practiced as instructed on the ground? And what are the social and economic impacts of prevention measures on communities and individuals? A team of researchers, including Constance Mackworth-Young and Rashida Ferrand from LSHTM, conducted a rapid qualitative study to better understand limitations and strengthen engagement in Zimbabwe’s efforts.
Local context and community beliefs are pivotal to the success of public health measures. However, these considerations are often sidelined in the early days of an epidemic. For COVID-19, the effectiveness of recommended behaviors like social distancing and hand hygiene depend on the reality of people’s living situations. In this study, researchers bring community member and health worker experiences to center stage.
Findings showed major gaps between policy and action. Study participants described an overload of information from social media and news channels but found it difficult to discern what was reliable. Social distancing efforts were reportedly inconsistent in public spaces and often deprioritized in the face of necessity, with people leaving home to obtain food, water, or basic income for their families. Generally, respondents regarded the ability to shelter in place as a privilege reserved for wealthier individuals and neighborhoods.
Among health workers, research revealed heightened perceived vulnerabilities and a lack of trust in the medical system. After the President’s COVID-19 declaration, doctors and nurses protested the insufficient availability of personal protective equipment, lack of safe water access, and no risk pay. Respondents expressed further concern over the neglect of other health services, including essential medicine and family planning provision, due to COVID-19.
Recommendations from this study emphasize a need for COVID-19 responses that reflect lived realities. To increase uptake of precautionary behaviors, the Zimbabwean Ministry of Health must address the social, financial, and resource obstacles that hinder community engagement. Researchers suggested multiple, more feasible measures. To offset the economic burden of staying at home and ensure reliable water access, basic supplies and cash transfers could be distributed. Within households, families could shield high-risk individuals and handmake masks. The paper concluded with a call to international donors to bolster the government’s finite resources by supplying personal protective equipment and relief packages.
The spread of COVID-19 presents severe repercussions to low- and middle-income countries such as Zimbabwe. Densely populated areas, high comorbidity rates, limited government finances, and inadequate intensive care capacity are key barriers to stemming COVID-19 transmission and averting excess mortality. These factors make adherence to protective measures challenging, and consequences could be catastrophic.
The LSHTM Viral podcast sheds further light on the toll of COVID-19 in African countries. In episode 20, Dr. Rashida Ferrand in Zimbabwe and Dr. Abdul Sessay in The Gambia weigh in on the high stakes and recent advancements. Listen to the LSHTM Viral podcast here.
- Sasha Baumann, A-Theme Student Liaison
If you enjoyed this article and would like to build a career in global health, we offer a range of MSc programmes covering health and data, infectious and tropical diseases, population health, and public health and policy.
Available on campus or online, including flexible study that works around your work and home life, be part of a global community at the UK's no.1 public health university.
