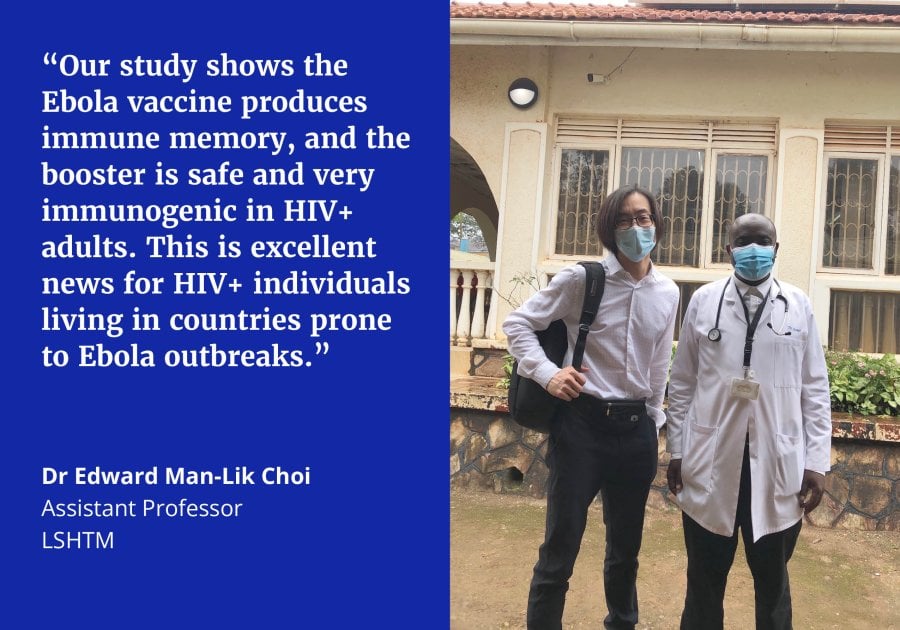
Photo above: Trial coordinators Dr Edward Choi (left) with Dr Ggayi Abu-baker Mustapher (right) at the MRC Masaka Field Station in Uganda.
Outbreaks and epidemics of Ebola virus have occurred in a number of countries in sub-Saharan Africa, including countries that also have a significant number of people living with HIV. Over the past 9 years, progress has been made in the development of vaccines to prevent Ebola infection. Following a number of clinical trials, several vaccines are now licenced for use in future outbreaks. Since HIV can impair the body’s ability to defend against infections and weaken the body’s response to immunisation, it is very important to evaluate vaccines in HIV infected people.
This recently completed study of an Ebola vaccine in HIV-positive participants is part of a series of Ebola vaccine trials conducted by the EBOVAC consortium. First launched in response to the West Africa Ebola outbreak in 2014-2016, the consortium aims to assess a two-dose Ebola vaccine regimen, Ad26.ZEBOV (Zabdeno®) as the first dose and MVA-BN-Filo (Mvabea®) as the second dose given 2 months later. In HIV-negative individuals, the vaccine regimen was found to be safe and to result in a good immune response.
An earlier study conducted in Uganda and Kenya in 2017 showed that the vaccine was also safe and produced good immune responses in HIV-infected adults. Our latest study followed up these participants and showed that more than 90% of them still had Ebola antibodies 4.5 years after vaccination. In addition, the study found that a booster dose of Zabdeno® given to these previously immunised participants with well-controlled HIV infection was also safe and resulted in very high level of antibodies 7 days after the booster vaccination, just like in uninfected individuals. This is good news for HIV-positive individuals living in countries prone to Ebola outbreaks. More work will be needed to see if this Ebola vaccine regimen/booster can also induce long-term immune responses in HIV-positive people who have less access to antiretroviral therapy or whose HIV infection is less well-controlled.
Additional Information
This study was sponsored by by the London School of Hygiene & Tropical Medicine (LSHTM) and carried out by the Kenya AIDS Vaccine Initiative (KAVI), Institute of Clinical Research in Nairobi, Kenya, and the Medical Research Council/Uganda Virus Research Institute (MRC/UVRI) and LSHTM Uganda Research Unit at Masaka, Uganda. The chief investigator and principal investigators are Professors Deborah Watson-Jones, Omu Anzala and Pontiano Kaleebu. The vaccines were manufactured and donated by Janssen Vaccines & Prevention B.V. (Johnson & Johnson) and the funding was provided by the Innovative Medicines Initiative 2 Joint Undertaking under grant agreement No 115854.
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.
