This Sickle Cell Life: voices and experience of young people with sickle cell
This Sickle Cell Life: voices and experiences of young people with sickle cell
Understanding the experiences of young people with sickle cell as they transition to adulthood and adult healthcare services.
Learn more about the project and the team, check out our publications and follow us on Twitter.
This collaborative research project, funded by the National Institute for Health Research (NIHR), Health Services and Delivery Research Programme, examines the experiences of young people with sickle cell as they transition to adulthood and move from using child to adult services.
Learn more about our findings dissemination day with patients, carers, campaigners and clinicians.
Recent updates
Events
Newsletter

This Sickle Cell Life is an NIHR-funded project run by DEPTH (Dialogue, Evidence, Participation & Translation for Health) researchers at the London School of Hygiene & Tropical Medicine.
The LSHTM team includes:
Professor Cicely Marston (Principal Investigator)
Dr Alicia Renedo (Research lead)
Dr Sam Miles (Research fellow)
Our sickle cell patient experts/parent experts include Cherelle Augustine, Patrick Ojeer and Nordia Willis.
DISCLAIMER:
This project was funded by the National Institute for Health Research Health Services and Delivery Research Programme (project number 13/54/25). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the HS&DR Programme, NIHR, NHS or the Department of Health. We thank all the participants who gave their time to the project, and Cherelle Augustine, Nordia Willis, and Patrick Ojeer for their expert input. We are grateful for the input of the National Institute for Health Research Clinical Research Network (NIHR CRN) and the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care Northwest London (NIHR CLAHRC NWL).
Recent updates
Events
Newsletter

What is This Sickle Cell Life?
This Sickle Cell Life is a collaborative research project at London School of Hygiene & Tropical Medicine (LSHTM), funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme. We have been examining the experiences of young people with sickle cell as they transition to adulthood and move from using child to adult services. The project aims to facilitate dialogue about how transitions into adult healthcare can be improved, including how to improve health services for people with sickle cell.
What is sickle cell disease and why are we focusing on young people?
Sickle cell disease is an inherited blood condition that causes severe pain episodes, with risk of stroke and severe infections. When young people with sickle cell disease first move to adult services, they are hospitalized a lot more than other age groups. We need to support them so that they are better prepared for adult services and self-management.
What happens when children become adults can affect their future lives. If you have a long-term condition you must learn to manage it yourself more as you get older. The healthcare services you use change as you transition to adult services. Those transitions do not always progress smoothly, which can have major effects on young people. This Sickle Cell Life has been exploring how young people with sickle cell disease move from using child to adult healthcare services.
How did we conduct the research?
This is a co-produced project. Our priority was to involve young people with sickle cell, and their parents and carers, every step of the journey, from the earliest planning stages.
Throughout the project, we have worked with people with sickle cell and a carer of a young person with sickle cell to design the study and think about the kind of issues we wanted to ask young people about. We also collaborated with these patient experts to analyse the data and think about the implications for practice. Having analysed the data together, we have co-authored an academic publication with them based on our findings, which you can read open-access. As well as involving young people and their parents and carers in developing the study – and writing research findings with patient experts – we worked with haemotologists, paediatricians, and quality improvement experts on developing the study, analysing findings, and working on how to get the findings into practice.
We conducted 80 interviews across England with 48 young people with SCD aged between 13 and 21. We took a sociological approach to look beyond the clinical realm into other areas relevant to transitions to adulthood such as education and social relationships.
What did we find?
We found that a key challenge for young people with SCD during transition relates to barriers to having a voice about their condition and practising patient expertise - knowledge of their body and of how the condition affects them – in interactions with others. On the one hand healthcare providers and parents/carers demand that the young person must learn more about their condition and body, and act responsibly to stay healthy. On the other, when the young person attempts to practise these new behaviours and use their patient expertise for instance by making requests about the care they receive, they are often disregarded, questioned or made to feel invisible. This feeling of not being listened to happened most within non-specialist healthcare settings during unplanned visits including Emergency care and on general hospital wards, as well as in social contexts such as school.
The main areas of concern for young people with regards to obstacles to receiving quality unplanned hospital care included pain relief needs not always being managed in a timely way; being ignored when asking for help with basic bodily care; and non-specialist staff not knowing enough about SCD. These healthcare experiences during the period of transition can negatively affect young people’s healthcare-related behaviour. Our findings suggest transitioning can involve young people with SCD developing mistrust in non-specialist hospital care. This can lead to avoidance tactics to stay out of hospital as much as possible. Going to hospital for unplanned care was viewed as a last resort, and participants pushed themselves to manage painful episodes at home despite knowing this could pose serious health risks. They also worried about the impact of their condition on their parents/carers. They learned how to protect parents/carers by concealing pain.
Our study also found that young people with sickle cell disease struggled to develop adult identities in healthcare transitions; that is, new ideas about how they should behave as adult patients. Young people saw themselves as in constant need of improvement to reconcile plural demands on the self; to produce bodily efficacy and stay healthy while working hard to become competent in other areas of their life, such as education, in order to become the type of productive adult they are hoped to be. Fulfilling educational demands is difficult for young people with SCD, who have to spend time in hospital, or who are in pain, or have to rest regularly to avoid painful episodes. At the same time, healthcare staff and parents push young people to take individual responsibility and become competent at self-management. The difficulties in trying to develop self-actualising adult identities whilst trying to be a disciplined adult patient can be played out in stigmatising identities including perceptions of 'laziness'.

What next?
Through this research we are contributing to knowledge of the neglected areas of both healthcare transitions and transitions to adulthood for young people with sickle cell. As well as providing valuable information for sickle cell advocacy organisations, clinicians, and improvements to NHS services, the co-produced outputs of this project are helping children and young people with sickle cell in their transitions from child to adult care. Read more about our participatory dissemination event.
Our project has shown that we need to work to educate non-specialist healthcare providers about sickle cell disease and address the stigma associated with use of pain relief medication. With more specific knowledge about sickle cell disease combined with a commitment to amplifying young people's voices and acting on their needs, non-specialist healthcare services will be better placed to respond to young people's needs and actively involve them as experts in their own condition.
We also need to educate the wider public, including those in educational contexts and anyone in contact with young people with sickle cell, about the condition and how it impacts young people's lives - for example, sickle-cell related fatigue and pain. If we do not address the wider social context of life with sickle cell, young people may continue to keep the condition private, not getting support and being misunderstood by society. This could pose challenges to achieving their life goals and have damaging effects on their health.
Where can I read more?
Our research findings are published on the Publications page, with straightforward summaries. All these articles are open access and free for anyone to read.
You can also follow the results published from This Sickle Cell life on our Twitter account, as well as learning about our wider work in healthcare involvement at our DEPTH Twitter account, DEPTH blog and DEPTH website.

Recent updates
Events
Newsletter
In this article we explore how young people with sickle cell disease experience healthcare during the period of transition – the time from when a young person prepares to move into adult healthcare services until the person is fully adjusted to adult services. We conducted 80 interviews across England with 48 young people with sickle cell disease aged between 13 and 21. We focused on their experiences of healthcare outside specialist sickle cell clinics, such as A&E. We found that young people reported problems with both the care they received in A&E during painful episodes, and in hospital wards as inpatients. They were not listened to by non-specialist hospital staff, nor recognised as experts in their own condition. They experienced delays in being given pain relief. Because of their experiences, young people tried to avoid going to hospital, attempting to manage their pain at home and going to hospital for a painful episode only as a last resort. Our study highlights the need for improvements to make services youth-friendly and to act on young people’s voices to ensure they are involved in shaping their own healthcare. We also argue that training staff in sickle cell disease-specific care is key to young people's well-being.
When young people move from child to adult health services they redefine their identities, but we don’t yet know enough about how these transitions shape identities. Our interviews with young people with sickle cell disease explored how they define new identities as they transition to adulthood. We show that health transitions are tricky for young people, who have to balance competing demands for self‐discipline: to stay healthy while working hard to become successful adults in other areas of their life. The development of adult identities for young people with SCD can be exhausting, involving relentless self-disciplining and self-monitoring in different aspects of life. They see themselves as in constant need of improvement. We conclude that it is crucial to create enabling spaces for young people to protect their health while still developing identities that help them achieve life goals.
In this paper, co-produced between academic researchers and people with lived experiences of sickle cell, we examine how young people with sickle cell disease try to use their expertise in their own condition during emergency hospital admissions and through encounters with non-specialist healthcare workers. Our qualitative research in England examined young people’s experiences of hospital encounters through repeat and one-off interviews. We show that young people’s expertise is sometimes undermined, including not being taken seriously when they report pain. They face barriers to care in non-specialist wards, particularly when they are alone with nobody to advocate for them. Although healthcare services encourage young people to take control of their health, in practice young people’s expertise is routinely ignored. To improve health service quality and young people’s needs, their own expertise must be better supported by healthcare providers.
Recent updates
Events
Newsletter

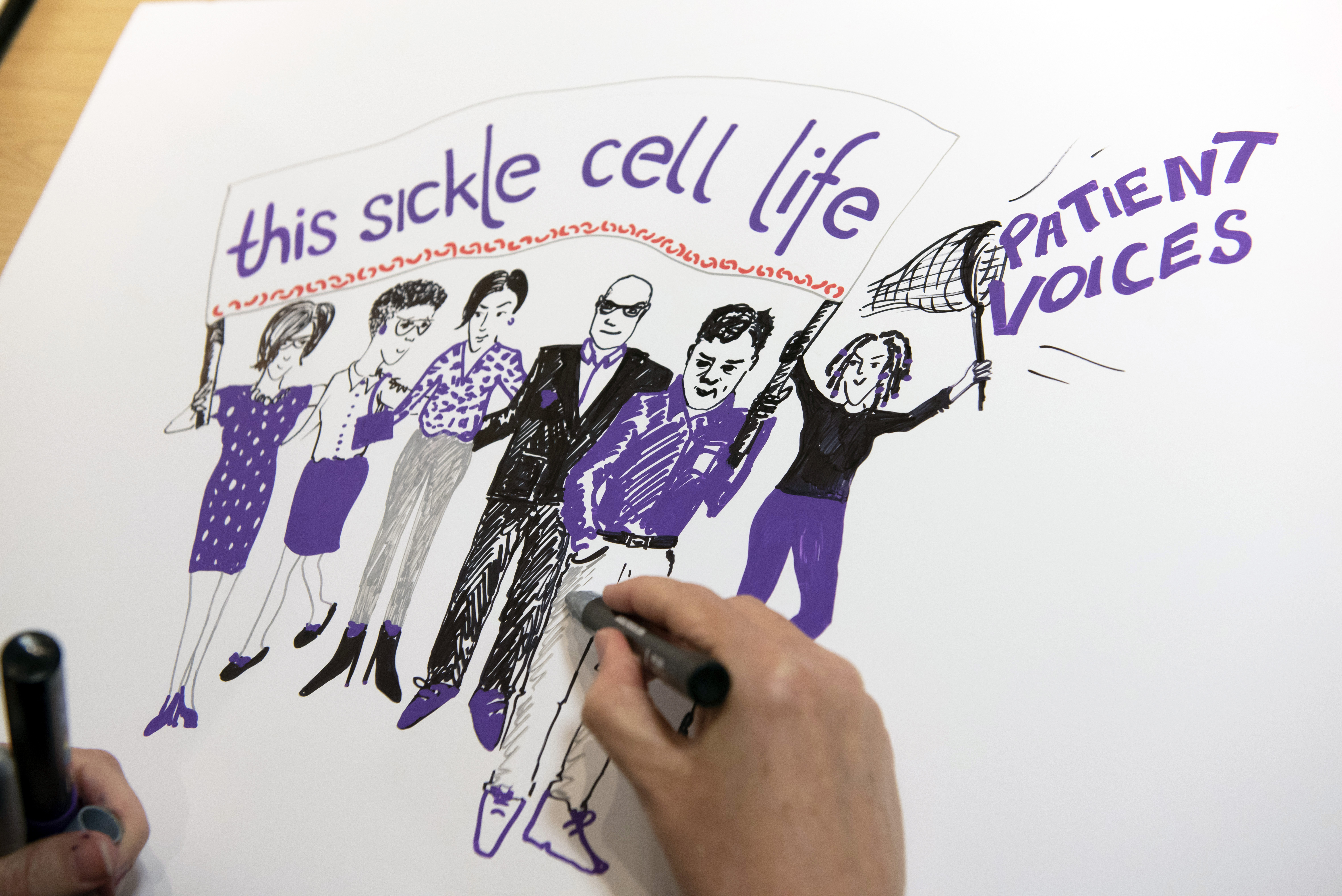
‘This Sickle Cell Life’ Participatory stakeholder event
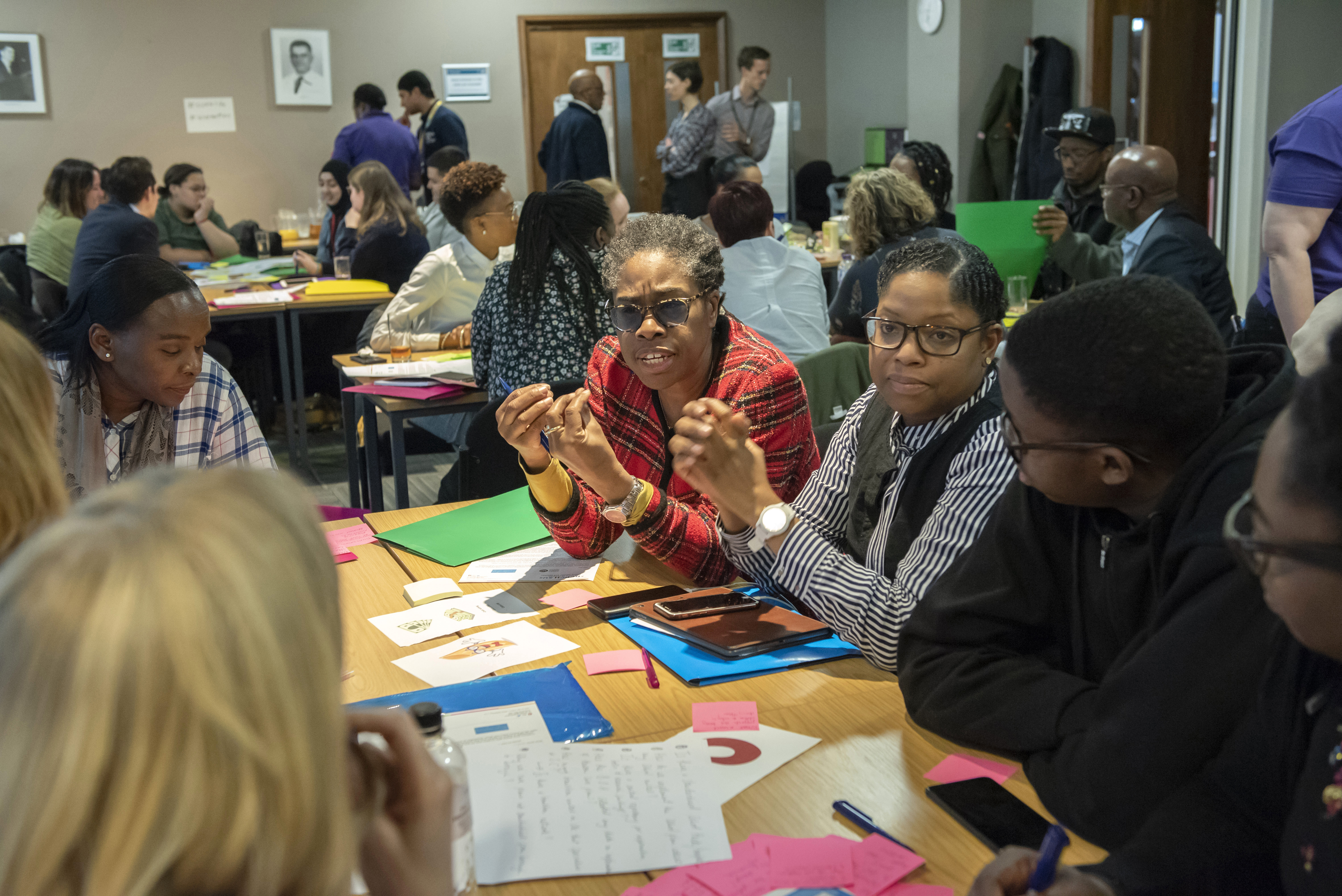
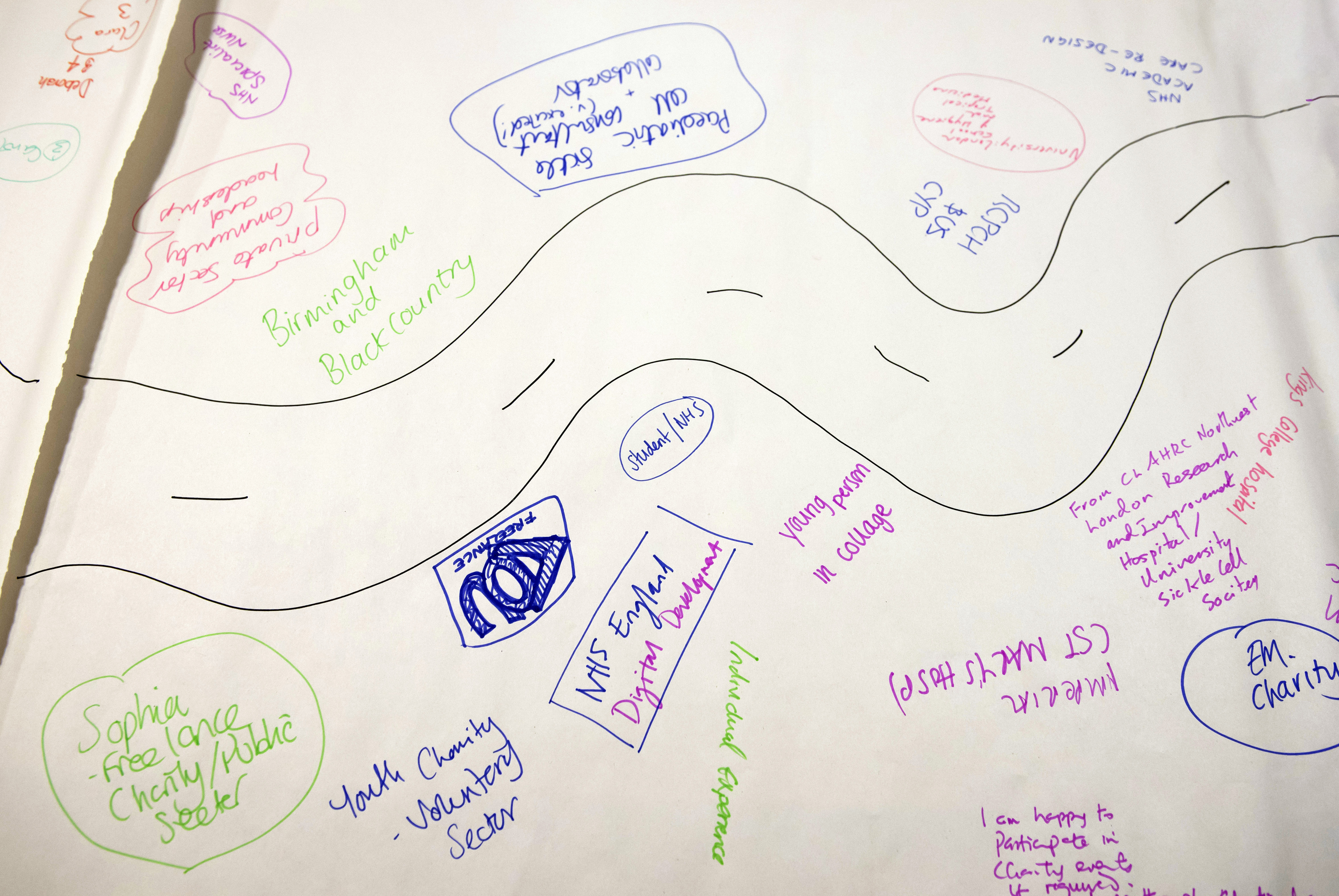
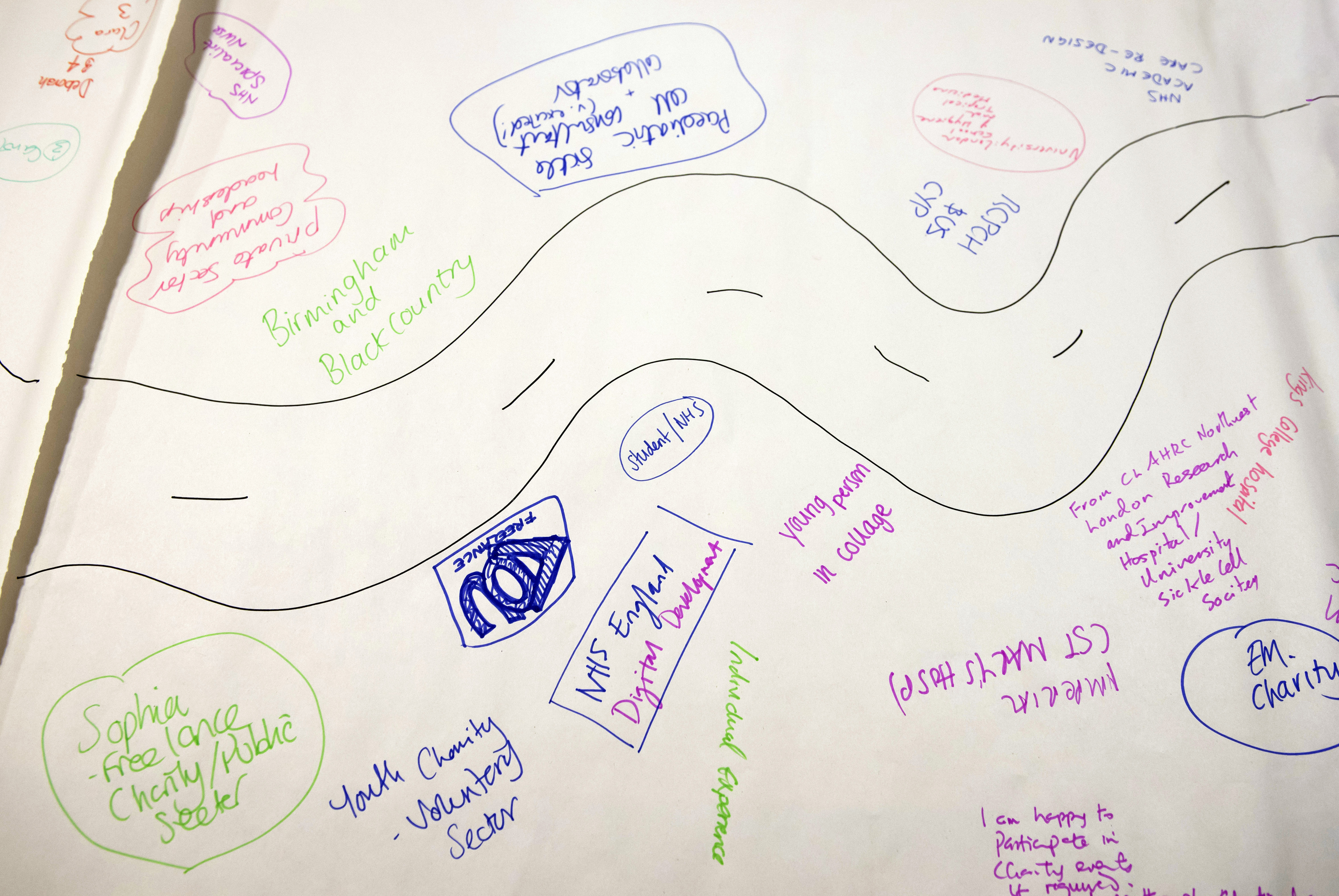
We ran a participatory event for ‘This Sickle Cell Life’ in April 2019, which provided us with an opportunity to engage directly with stakeholders, including young people with sickle cell disease and other long term and/or chronic conditions, parents and carers, sickle cell charity staff, policymakers, clinicians and researchers.
Working with the RCPCH &Us involvement team at the Royal College of Paediatrics & Child Health (RCPCH), we asked attendees to reflect on the research findings and draw on their different backgrounds and experiences to work together to co-produce ideas for resources to improve transitions that can be targeted to different stakeholders involved in the care of young people with SCD.

The participatory workshop fostered an extended dialogue between young people, carers and specialists with key stakeholders who we specifically wanted to influence such as A&E doctors and non-specialist healthcare providers and educational staff. They collaboratively reflected about the implications of our qualitative research findings for practice and co-produced ideas to improve transitions for young people with SCD at a personal, community and strategic level.
Attendees made their own pledges to support the future of ‘This Sickle Cell Life’. The event allowed us to reflect on the implications of our findings for practice, and in some cases turn our research findings into action to improve experiences of young people with sickle cell disease. The event was positively evaluated across the range of attendees. Evaluation feedback from non-specialist NHS clinicians was also positive: one respondent pledged to improve hospital emergency department training; another wrote of their intention to amplify the voices of young people at their emergency centre when designing care approaches.