
Baby in the neonatal unit of a hospital in Malawi. Credit: NEST360, Rice University
IMPRESS: Innovative Management PRactices to Enhance hoSpital quality and Save lives in Malawi
Examining whether enhanced hospital management practices can drive improvements in newborn survival and the quality of clinical care in Malawi
IMPRESS (Innovative Management PRactices to Enhance hoSpital quality and Save lives in Malawi) focuses on hospital management in Malawi. Building on an existing platform, Newborn Essential Solutions & Technologies (NEST360), we are identifying practical ways to enhance management practices in hospitals in Malawi, to improve quality of care and reduce newborn deaths. We are also strengthening the capacity and capability of the next generation of health systems researchers.
This is a four-year NIHR-funded project that started in October 2020. At the core of the research is an equitable partnership between Kumuzu University of Health Sciences and London School of Hygiene & Tropical Medicine. We are working with the Ministry of Health and other stakeholders to generate high quality evidence that has direct relevance for policy and practice in Malawi, the African region, and beyond.
We are a multi-disciplinary team of health system researchers, epidemiologists, health economists, social scientists, clinicians, implementation scientists and statisticians.
We are addressing what are three fundamental gaps in knowledge. First, until recently, we did not have the tools to measure the hospital adoption modern management practices. Building on recent advances, we are adapting and validating tools to Malawi to measure management practices. Second, no interventions to enhance hospital management practices have been rigorously evaluated. Working in partnership with the Ministry of Health, experts and other key partners, we are co-designing a management intervention with a view to evaluating it in a randomised controlled trial and other complementary methods. Third, it is rarely possible to measure lives saved in such health systems research.
By building on the existing NEST360 network of 36 hospitals with detailed patient level information on newborns admitted to hospital, we are examining which management practices matter most for quality of care.
We strengthen research capacity through formal postgraduate training (PhD and MSc), mutual learning during the research, skills training, and mentorship.
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk

Project rationale
Every year 2.5 million newborns die. Most of these deaths happen in hospital and could be prevented. Babies in their first 28 days of life represent some of the most vulnerable users of the health system, as they can die quickly. Malawi has been one of the fastest progressing countries in Africa for newborn survival. Now that most births happen in health facilities, there is an urgent need to improve hospital care for newborns and their families.
Health technologies and skilled clinical staff are a necessary ingredient for improving survival of small and sick babies. However, in practice, babies do not always get these clinical interventions even when resources are available. Commonplace problems, such as drug stockouts, absent staff, and power outages, may be due to organisational failings that are rooted in poor management. Improving management practices – so that hospitals effectively manage staff, drugs and medical supplies, have sound financial management and are data-driven in how they make decisions – offers the potential to turn the situation around.
Recent studies indicate that management practices – in the areas of human resource management, performance monitoring, target setting and operations – may be a driver of quality care but there are few relevant studies in low- and middle-income settings, especially ones with enough data on patient mortality.
Research
Building on an existing platform, Newborn Essential Solutions & Technologies (NEST360), we are identifying practical ways to enhance management practices in hospitals in Malawi. IMPRESS aims to examine whether enhanced management practices can improve health outcomes and clinical quality for newborns in hospitals. A multi-disciplinary team from Kumuzu University of Health Sciences and LSHTM will address the following main objectives:
- Adapt and validate measures of hospital and district management practices
- Examine the association between management practices and quality of clinical care, and its variation by facility characteristics
- Co-design a problem-focused hospital management intervention and scalable delivery model
- Evaluate effectiveness of the intervention on neonatal mortality and secondary outcomes (including hospital-acquired infections) through a cluster randomised trial
- Assess the intervention’s acceptability, fidelity, and mechanisms through multi-methods research and estimate its cost-effectiveness
Capacity strengthening
IMPRESS will generate novel evidence on hospital management practices, with two-way skills transfer between the UK and Malawi, strengthening capacity of health systems researchers, hospital staff and district health officials. We strengthen research capacity through formal postgraduate training (PhD and MSc), mutual learning during the research, skills training, and mentorship.
Partnership
IMPRESS is a collaboration between the Kumuzu University of Health Sciences, and London School of Hygiene & Tropical Medicine. We are working in close partnership with NEST360, the Government of Malawi’s Ministry of Health, and other stakeholders to inform policy to the benefit of neonates at high risk in Malawi, and beyond.
We work closely with LSHTM’s Centre for Health Economics in London and the Centre for Maternal, Adolescent, Reproductive, & Child Health.
Impact
Ensuring that the study findings have maximum impact is given high priority by all partners in the research team. The planned outputs from the research include:
- Validated tools to measure management practices at the hospital and district level
- Novel data on the extent to which hospitals adopt management practices and evidence on which practices matter for quality
- Co-designed hospital management intervention based on a well-articulated theory of change and developed with scalability in mind
- Rigorous evidence in a low income setting on the effectiveness of a hospital intervention to improve management practices, quality of care and patient outcomes
- Process findings on implementation, mechanisms, context and costs, to inform scale-up and generalisability to other countries
- Capacity strengthening of a cadre of management trainers with capability to scale up intervention, hospital clinicians and managers, and health system researchers
We focus on four key groups of users. In addition, as these groups act on the research findings, there is clear potential for neonates to benefit from improved quality of care in hospitals across the whole of Malawi:
- National stakeholders. They include national and district government bodies, professional associations and NGOs
- Hospital managers and clinicians. We are engaging early with this key group of users through zonal sensitisation workshops to maximise ownership and input into the design
- International funders. We are leveraging our long-standing relationships with international stakeholders and we will coordinate closely with NEST360 in communicating findings through its network in Kenya, Tanzania, and Nigeria
- Academic community. We aim to publish in a range of academic journals and are committed to ensuring open access. We will present findings at conferences and via webinars
Funding
This project (NIHR131237) is funded by the National Institute for Health Research (NIHR) using UK aid from the UK Government to support global health research. The views expressed on the website are those of the author(s) and not necessarily those of the NIHR or the UK Government.
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk

A multi-disciplinary team from the Kumuzu University of Health Sciences and LSHTM will address the following interlinked objectives (click on each one for more information):
- 1) To adapt and validate measures of hospital and district management practices
-
Formative qualitative research and psychometric performance assessment will generate validated tools to measure management practices.
This objective falls under the formative phase of research. We first identify and describe the types of management-related practices in hospitals and district health offices that may affect the quality of clinical care. Through in-depth interviews with hospital managers, clinicians and district health officials, we are exploring their understanding of what good management looks like in their setting, what practices are expected and implemented, perceptions of what management practices are important for supporting the provision of clinical care, and the attributes of effective leadership in a hospital setting.
An important part of the formative phase is to theorize how management practices may affect quality of care. Here we draw on causal loop diagrams, which are ideal for providing a blueprint for complex systems by representing important, non-linear feedback and relationships that further our understanding of how these systems operate. We undertake “group model building” sessions involving doctors, nurses and managers to map out – with the help of a causal loop diagram – the management-related causes of poor quality of care in the hospital.
Informed by these data and a review of existing instruments, we develop and implement a new survey tool to quantitatively measure the adoption of management practices in 36 hospitals. The survey includes a combination of interview with hospital managers, direct observation, and review of facility records. Using the cross-sectional survey data on management practices collected in the hospitals, we use psychometric methods to assess the acceptability, reliability and validity of the tool.
- 2) To examine the association between management practices and quality of clinical care
-
Data on management practices linked to patient level measures of clinical quality will provide observational evidence on which practices matter for quality.
This objective examines the association between hospital management practices and clinical quality, and its variation by facility characteristics. Study outcomes include neonatal outcomes, such as all cause in-hospital mortality, and clinical care processes for newborns, such as adherence to essential interventions for sick babies. The observational study makes use of the cross-sectional data on management practices collected in the first objective and links to these to the NEST360 patient level data. The latter is a de-identified prospective dataset on every newborn admitted to a newborn care unit in study hospitals containing information on the newborn’s admission status, maternal, birth and infant details, observations and nursing care, microbiology and labs, interventions and discharge outcome.
Analyses examine associations of hospital and district management scores with clinical quality. The primary outcome is all cause in-hospital mortality. Secondary outcomes are: birth weight standardized mortality, adherence to essential interventions for sick newborns (e.g. neonates <2500g who get kangaroo mother care); and neonates with hospital-acquired infections. further analyses explore the relative importance of individual management practices and sub-group differences with respect to hospital sector and level.
- 3) To co-design a problem-focused hospital management intervention and scalable delivery model
-
Stakeholder workshops that draw in national and international expertise will result in a theory-driven intervention to enhance hospital management practices.
Intervention development follows MRC guidance on complex interventions, including the need to identify relevant literature, develop the intervention around a credible theory of change, and consider implementation at an early stage. The intervention development draws on practical guidance on the importance of middle-level principles (e.g. support factors, derailers, safeguards) and more specific theoretical insights from the quality improvement literature (e.g. lean, six sigma, plan-do-study-act-cycles). It is also informed by early findings from objectives one and two – including the causal loop diagram derived from the model building workshops. We facilitate an inclusive process which brings together key stakeholders to co-design the intervention, including the Ministry of Health’s Quality Management Directorate, hospital managers and neonatal unit clinicians, and parent and community representatives. The output from this process is a co-designed hospital management intervention that is based on a well-articulated theory of change, thickened with information about the local setting in Malawi, and developed with scalability in mind.
- 4) To evaluate effectiveness of hospital management intervention on neonatal mortality and secondary outcomes (including hospital acquired infections)
-
A cluster RCT will generate evidence on the effects of enhancing hospital management practices on patient outcomes and clinical quality.
We evaluate the effectiveness of the hospital management intervention on neonatal mortality and secondary outcomes through a cluster randomised controlled trial. Since NEST360 is being implemented in all the study hospitals, we are testing the hypothesis that resources (medical devices, clinical training, quality improvement visits) in combination with supportive management practices can improve quality. The study outcomes include in-hospital mortality of newborn admissions (primary) and secondary outcome measures of clinical quality and uptake of management practices.
- 5) To assess acceptability, fidelity, and mechanisms of effect and estimate cost-effectiveness
-
A process evaluation and cost-effectiveness analysis will inform scale-up in Malawi and generalisability of the trial findings to other countries.
We conduct a process evaluation based on MRC guidance on complex interventions and realist evaluation principles, to address the following questions. Is the intervention implemented as intended? Is it acceptable to hospital staff? Do the mechanisms that underpin the intervention work, and if not, why not? How does context affect the success or failure of the intervention? Is it value for money? The process evaluation – particularly the focus on mechanisms – will be guided by the theory of change developed in the third objective. We draw on in-depth interviews, routine programme data and economic cost data.
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk
The IMPRESS team see mutual capacity strengthening as vital for a successful collaboration, and a key foundation of an equitable partnership, building on the strong traditions of Kumuzu University of Health Sciences and LSHTM in this area.
We aim to strengthen capacity and capability at both the individual and institutional level, with a view to enhancing IMPRESS research, its communication and policy impact, and the long-term futures of the individuals and institutions involved.
Our capacity strengthening strategies based on the following principles:
- The strategy is developed collaboratively across the team
- It covers individual researchers at all levels, team administrators, our research organisations and, where appropriate, our policy and implementation partners
- It is informed by systematic needs assessments
- Opportunities are allocated in a transparent and equitable manner
- We emphasise opportunities for mutual learning across the team
- We monitor and evaluate our progress
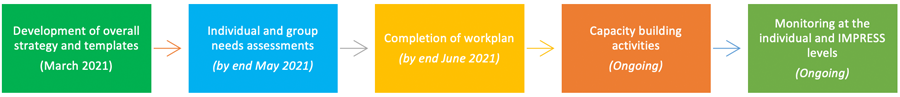
The scope of our capacity development activities includes (i) formal post-graduate training; (ii) knowledge exchange during regular meetings and workshops; (iii) mentoring; and (iv) targeted training sessions. We follow these five key stages:
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk

Timothy
Powell-Jackson
Professor in Health Economics

Catherine
Goodman
Professor

Joy
Lawn
Professor of Maternal, Reproductive and Child Health

Charlotte
Ward
Research Fellow in Health Economics

Christian
Bottomley
Professor in Medical Statistics
Carla Cretan
Project Manager

Victor Mwapasa
Professor of Epidemiology and Public Health

Linda Nyondo-Mipando
Lecturer in health Systems and Policy
Wanangwa Chimwaza-Manda
Social Scientist
Andrew Kumitawa
Statistician
Vincent Phiri
Data Manager
Florence Mshali
Project Manager
Monica Malata
NIHR Academy Member (PhD)
Elias Phiri
NIHR Academy Member (MSc)
Madalitso Tambala
NIHR Academy Member (MSc)

Queen Dube
Professor & Head of Department of Pediatrics at Queen Elizabeth Central Hospital
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk
Project publications
Ward, C., Phiri, E.R.M., Goodman, C., Nyondo-Mipando, A.L., Malata, M., Manda, W.C., Mwapasa, V. and Powell-Jackson, T., 2024. What is the relationship between hospital management practices and quality of care? A systematic review of the global evidence. Health Policy and Planning, p.czae112.
Mangwiro, L., Misyenje, J., Iroh Tam, P.Y., Kawaza, K. and Nyondo Mipando, A.L., 2024. Determinants of neonatal mortality among hospitalised neonates with sepsis at Queen Elizabeth Central Hospital, Blantyre, Malawi: A mixed-methods study. PLOS Global Public Health, 4(12), p.e0004059.
Research briefs, presentations and posters
- Hospital Management in Malawi: What areas of management are most in need of improvement?
- Hospital management in Malawi: Development and assessment of a management survey tool
- Does hospital management matter for quality of care? A systematic review of the global evidence (iHEA Congress presentation, July 2023)
- Does hospital management matter? Evidence on the relationship between hospital management practices and the quality of newborn care in Malawi (iHEA Congress poster, July 2023)
Research and implementation tools
- IMPRESS hospital management survey tools (baseline)
- IMPRESS hospital management survey interviewer guide (baseline)
- IMPRESS hospital management survey tools (endline)
- Small and sick newborn care implementation tools (NEST360 and UNICEF)
Related publications
Powell-Jackson T, King J, Makungu C, Quaife M, Goodman C. Management practices and quality of care: Evidence from the private health care sector in Tanzania. The Economic Journal, 2023
Rao SPN, Minckas N, Medvedev MM, Gathara D, …Lawn JE; COVID-19 Small and Sick Newborn Care Collaborative Group. Small and sick newborn care during the COVID-19 pandemic: global survey and thematic analysis of healthcare providers' voices and experiences. BMJ Glob Health. 2021 Mar;6(3):e004347. doi: 10.1136/bmjgh-2020-004347. PMID: 33716220.
Minckas N, Medvedev MM, Adejuyigbe EA, …Lawn JE; COVID-19 Small and Sick Newborn Care Collaborative Group. Preterm care during the COVID-19 pandemic: A comparative risk analysis of neonatal deaths averted by kangaroo mother care versus mortality due to SARS-CoV-2 infection. EClinicalMedicine. 2021 Feb 15;33:100733.
Powell-Jackson T, Purohit B, Saxena D, Golechha M, Fabbri C, Ganguly PS, Hanson K. Measuring management practices in India's district public health bureaucracy. Soc Sci Med. 2019 Jan;220:292-300.
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk
IMPRESS is strengthening capacity, in part, through its support for students studying at the London School of Hygiene and Tropical Medicine in the UK and the Kamuzu University of Health Sciences in Malawi. Learn more about our fantastic students.
- Monica Malata (PhD candidate)

“I look forward to pursuing a career in health financing after I complete my PhD.”
I am a PhD student at LSHTM, studying district-level healthcare priority setting and resource allocation processes and their implications on neonatal healthcare prioritisation in Malawi. Specifically, I am tracking expenditures on neonatal healthcare and analysing the funding flows; and evaluating priority-setting processes and using causal loop diagrams to assess factors affecting the optimal prioritisation of neonatal health. Additionally, I am costing IMPRESS hospital management interventions aimed at improving neonatal health.
I expect to estimate the neonatal health expenditure as a proportion of total health expenditure and map out the major sources of funding for neonatal health. I will also produce a causal loop model of the factors influencing optimal prioritisation of neonatal health, showcasing the dynamic and interconnected nature of health system elements. Ultimately, I seek to explain, evaluate, and inform priority setting and resource allocation processes.
- Charlotte Ward (PhD candidate)

“A highlight of working on the IMPRESS project has been the opportunity to be a part of a multi-disciplinary team that fosters mutual capacity strengthening and encourages everyone to contribute their unique perspective.”
I am doing a staff PhD at LSHTM. My research project explores how to measure management in hospitals and investigates its relationship with neonatal quality of care in Malawian hospitals.
A key learning has been the process of defining and quantitatively measuring management. As part of this, we developed the Malawi Hospital Management Survey and tested its performance. We learned that the tool is acceptable to mangers in Malawian hospitals, and is both reliable and valid. We also tested several different approaches to quantitatively measuring management and learnt about their merits and drawbacks. Additionally, we aim to contribute to the evidence base around the cross-sectional relationship between management and quality of care in a low-resource setting. Finally, following the implementation of a 12-month management intervention in Malawian hospitals, we hope to understand the key mechanisms that can facilitate improvements in quality of care for small and sick neonates.
- Elias Phiri (MSc in Public Health)

“The IMPRESS project and team has propelled my growth in implementation science.”
I completed my MSc in Public Health at LSHTM with support from IMPRESS. My project is entitled ‘From Policy to Practice: Assessing the People Centred Care Policy in Neonatal Health at Chiradzulu District Hospital’. It is a case study approach in assessing the uptake of people-centered care policy in neonatal health in Malawi.
My study revealeda lack of single policy for people-centered care in Malawi showing that the concept is presented differently in several guiding documents. There were existing discrepancies in the framing of people-centered care as a policy, its targets, and activities timelines across various documents. Furthermore, there was also lack of a clear resource allocation framework and a communication strategy for ensuring people-centered care enhancement. The study showed existence of multiple people-centered care players, however, most of them lacked capacity. In general, it was noted that people-centered care interventions have not been widely implemented as intended.
- Madalitso Tambala (MSc in Public Health)

“My research dives into how savvy, data-driven hospital management practices can turn long stays into swift departures for our tiniest patients.”
I am studying for the MSc in Public Health at LSHTM. My research project focuses on the application of statistical methods to examine the association between hospital management practices and the length of stay of neonates in hospitals in low- and middle-income countries (LMICs), with a particular focus on Malawi.
By using well-curated data on hospital management practices and length of stay, this research aims to unravel the association between the main domains of hospital management practices applied in Malawian hospitals and their relationship to the length of stay of neonates. My project builds on research done in high-income countries, where it has been observed that hospitals whose management practices include well-defined, technology-driven, and evidence-based clinical protocols for neonatal care tend to have more efficient care pathways, potentially reducing the length of stay. The uniqueness of my project is that it not only takes into consideration a larger spectrum of hospital management practices common in LMICs but is also quantitative, as opposed to the mostly qualitative studies done in LMICs. By understanding the association between hospital management practices and length of stay, the findings of the project have the potential to facilitate healthcare system optimization, thereby freeing already constrained healthcare resources in Malawi.
- Wongani Mtabayira Nyondo (MSc in Epidemiology)

“Quality data drives evidence-based interventions and actions by management.”
I am studying the MSc in Epidemiology at Kamuzu University of Health Sciences. My project, supported by IMPRESS, is about assessing the quality of neonatal data and how management utilize the neonatal data collected. It uses a mixed method cross sectional study done at two district hospitals in southern Malawi, namely Thyolo and Chikwawa District hospitals with the aim of assessing the completeness of the data in the ward register and associated factors, accuracy and its associated factors, service delivery improvement, enablers, and challenges in service delivery improvement implementation.
The study found that the ward register data had a completeness rate of 59%. The possible issues that could affect accuracy were poor documentation of the data, shortage of stationery and poor data management. Introduction of death audits and reviews, lobbying for additional resources and improving neonatal management of care were service delivery improvements that were found in the study. The study found that availability of support systems, teamwork and trained staff help the implementation of service delivery improvements. On the hand, inadequate resources and health worker attitude affected the implementation of service delivery improvements.
- Nelson Maloni Banda (MA in Business Administration in Health Systems Management)

“I coordinated and monitored the IMPRESS management intervention adoption at Ntcheu DHO, resulting in a 78.6% improvement in overall management score by visit ten.”
I am studying for the MA in Business Administration in Health Systems Management at Kamuzu University of Health Sciences. My project, supported by IMPRESS, is a longitudinal retrospective quantitative study assessing trends in the adoption of multi-faceted hospital management practices in support of sick neonates in Malawi.
The analysis has demonstrated a significant improvement in the management practices among ten secondary hospitals in the intervention arm following the adoption of the IMPRESS intervention. Management practices under service delivery in the neonatal unit domain have contributed substantially to the changes in the overall management score.
- Lucky Mangwiro (MSc in Global Health Implementation)

“With the experience gained during this course, my focus is to specialize in global health policy and clinical research in order to provide evidence-based solutions hence able to achieve the Malawi 2063 agenda.”
I have completed studying for the MSc in Global Health Implementation at Kamuzu University of Health Sciences. My research project, supported by IMPRESS, was entitled ‘Determinants of neonatal mortality among hospitalized neonates with sepsis at Queen Elizabeth Central Hospital, Blantyre, Malawi: a mixed methods study’.
The study findings were that gestation age (weeks) and number of days spent in the hospital were the most predictive risk factors for neonatal mortality among neonates with sepsis in the multivariable logistic regression analysis model. Prematurity, mother's years (mom's age), birth weight, gestational age, type of birth (single vs multiple), and number of days spent in the hospital were highly correlated predictors of neonatal mortality among neonates with sepsis in the univariable logistic regression model. The qualitative inquiry showed that maternal behavioural; reporting late to hospital, and cultural and religious beliefs contributed to documented clinical outcomes.
Recent updates
Events
Newsletter
Contact us
Timothy Powell-Jackson
Professor of Health Economics
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Victor Mwapasa
Professor of Epidemiology and Public Health
Kumuzu University of Health Sciences
Carla Cretan
IMPRESS Project Manager
Faculty of Public Health and Policy
London School of Hygiene & Tropical Medicine
Carla.Cretan@lshtm.ac.uk
