This article is part of the Decade of Health campaign from organisations across the UK – including LSHTM – who are working to make the world healthier and safer through innovation and collaboration. Check out decadeofhealth.co.uk and find out more about how research institutes are bringing together the world’s greatest scientific minds to develop solutions to challenges such as AMR, and leading the way for science and innovation.
1. We’re not looking for antibiotics in bread mould anymore… artificial intelligence is accelerating the search for new drugs.
There’s no doubt that antibiotics have revolutionised medicine, but the first was discovered completely by accident. In 1928, Alexander Fleming left a bacterial culture on his lab bench while he went on holiday. When he returned, he found that where a mould had contaminated the plate, bacteria wouldn’t grow – he named the chemical produced by the mould penicillin.
The first bacteria resistant to penicillin, however, were reported as early as 1940, and since then scientists have been in an arms race with germs, scrambling to develop new and better drugs. Recently, they’ve been losing the battle, with only 15 new antibiotics approved this century, and 700,000 people dying from drug-resistant infections each year.
New technologies could be a game-changer for drug discovery. At LSHTM, a team led by Dr Nick Furnham is using computational techniques to understand how genetic changes in microbes give them the ability to evade drugs.
Armed with this information, they are developing artificial intelligence tools that can rapidly screen thousands of chemicals for their antimicrobial activity, allowing them to identify potential new medicines.
They are even using AI to design completely new drugs, incorporating features that reduce the likelihood of resistance arising in bacteria, so they will hopefully stay effective for many years to come.
2. It’s not just bacteria that develop resistance… viruses, fungi and parasites are all getting more dangerous.
Bacteria often receive the most attention when it comes to drug resistance, but they aren’t the only microscopic organisms outsmarting our medicines.
This year, the World Health Organization rebranded its annual campaign from World Antibiotic Awareness Week to World Antimicrobial Awareness Week, reflecting the growing need for a unified response to these threats.
Alarmingly, there are now forms of HIV, a viral infection, spreading around the world that continue to multiply in the presence of antiretroviral drugs. And decades of progress in malaria control are at risk due to drug resistance developing in the single-celled malaria parasite, Plasmodium falciparum.
At LSHTM, our malaria labs are conducting research to identify the genetic changes that allow this parasite to withstand anti-malarial drugs. Dr Khalid Beshir has even developed approaches to detect strains of P. falciparum that have evolved to become ‘invisible’ to standard malaria rapid diagnostic tests, meaning the parasite evades detection – and treatment.
Understanding the ingenious ways these microbes are outmanoeuvring doctors will be critical to fighting non-bacterial infections, which cause some of the deadliest diseases in the world.
3. AMR doesn’t only arise in humans… livestock, and even crops, can be sources of superbugs.
We’ve all heard the advice from our doctor to ‘finish your course of antibiotics’ and probably know that we shouldn’t take penicillin for a sore throat. But it’s not only the misuse of antibiotics in people that results in resistant infections – AMR occurs in animals too.
Estimates for the amount of antibiotics used in agriculture range from around 63,000 to over 240,000 tonnes each year – on a scale at least equivalent to use in humans. In livestock, they are mostly used speed up growth and prevent disease, rather than to treat specific infections. These drugs can contaminate the environment and end up in the food chain, or resistant infections can develop in animals that jump into people.
And if you thought going vegan was the answer, we’ve got some more bad news.
There’s growing evidence that the antibiotics used to treat people and animals can contaminate food crops. This could pose a threat to human health by promoting the growth of drug-resistant microbes on the crops, or possibly even in the human body after eating them.
At LSHTM, Professor Jeff Waage and Dr Ariel Brunn are currently researching the potential transmission pathways from plants to humans, to work out how we can avoid growing superbugs alongside our veggies.
4. AMR isn’t just a public health concern... it also has huge economic costs.
The more pessimistic among us believe we’re heading for an AMR apocalypse, where our ability to treat diseases returns to that of the early 20th century, and minor injuries and infections become a death sentence once again. While this worst-case scenario is unlikely any time soon, the global death toll from drug-resistant diseases is rapidly rising and is certainly the most serious consequence of AMR.
Another worrying, but less well-known, outcome of AMR is the economic cost. The current COVID-19 pandemic has highlighted the economic impact a health crisis can have – UK GDP fell a record 20.4% in the second quarter of this year, compared with the previous three months.
AMR is likely to have similarly dire consequences for the global economy, albeit in a more gradual way. Falling labour productivity from illnesses that are harder to treat, coupled with rising healthcare expenditure, is already placing a strain on low-income countries.
AMR also has the potential to make the treatment of livestock more difficult, which could financially burden farmers and food systems globally.
At LSHTM, Dr Nichola Naylor is working with the World Health Organization and agriculture research institutes, such as CGIAR, to understand these economic costs and model their future impact.
This research aims to reveal the financial crisis lurking in the shadow of a health crisis, allowing governments to plan for, and mitigate, the economic impact. It’s hoped that if the prospect of an AMR apocalypse wasn’t enough motivation to tackle the AMR problem, perhaps a look at our future balance sheet will be.
5. The COVID-19 pandemic is driving AMR infections up… or maybe down… around the world.
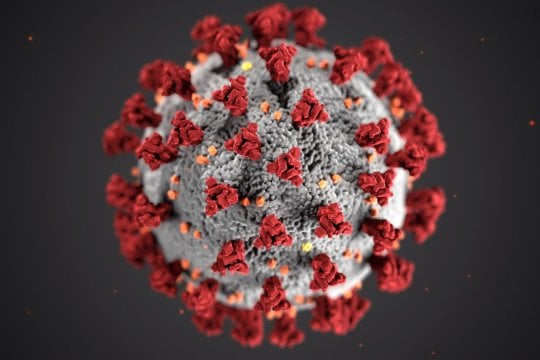
AMR has long been a contender for the world’s biggest global health challenge. Until this year, that is. It’s fair to say AMR has lost its podium position to the coronavirus pandemic.
Perhaps surprisingly, the two health challenges are in fact linked. However, scientists remain divided on whether the pandemic will increase or decrease numbers of infections with AMR pathogens.
On the one hand, there is evidence that the pandemic is increasing the use of certain antimicrobial drugs around the world, because hospitalised patients with COVID-19 are often prescribed antibiotics to prevent or treat secondary infections. Disruption to healthcare services could also fuel an increase in people self-medicating and misusing antimicrobials. Both of these are likely to drive up the number of resistant infections.
Other scientists, however, believe that measures to reduce the spread of COVID-19, such as handwashing, social distancing and reduced air travel, could temporarily slow the spread of other infectious diseases, reducing AMR.
The reality is likely to not be so clear cut: for certain drug-bug combinations in some settings, COVID-19 will result in more AMR, in others less. At LSHTM, a team led by Dr Gwen Knight is busy gathering the evidence as it emerges, to reveal the complex relationship between these two ongoing health crises.
LSHTM's short courses provide opportunities to study specialised topics across a broad range of public and global health fields. From AMR to vaccines, travel medicine to clinical trials, and modelling to malaria, refresh your skills and join one of our short courses today.