There is increasing availability of routinely collected data, including linked and anonymised electronic health records, administrative data, and drug and disease registries. The EHR Research Group at LSHTM comprises a wide range of epidemiologists, statisticians, and clinicians with extensive experience analysing real-world data from around the world.
Our work covers a broad spectrum including disease aetiology, safety and effectiveness of medications, vaccines and surgery, environmental influences, and health services research. We have particular interest in developing and applying optimal research methods, including both observational and interventional approaches.
There is increasing availability of routinely-collected data, including linked and anonymised electronic health records (EHRs). The overarching aim of the EHR Research Group is to capitalise on research opportunities offered by the availability of routinely-collected data, bringing methodological rigour to provide real-world evidence for important questions regarding human health.
The EHR Research Group at LSHTM comprises a wide range of epidemiologists, statisticians, and clinicians with extensive experience analysing real-world data from around the world. We have a diverse programme of work using a range of anonymised data sources. These include the UK Clinical Practice Research Datalink (CPRD) based on primary care records, the OpenSAFELY platform, secondary care records including Hospital Episode Statistics, administrative data including those provided by the Office for National Statistics, drug and disease registries, the UK Biobank, and numerous international data sources.
Our work covers a broad spectrum including disease aetiology, safety and effectiveness of medications, vaccines and other medical products, environmental influences, and health services research. Disease areas are similarly diverse, with major interests in a range of both non-communicable and communicable diseases. We have particular interest in developing and applying optimal research methods, including both observational and interventional approaches.
Our research is funded by a range of different government bodies, charities, and companies. These include the Wellcome Trust, Medical Research Council, National Institute for Health Research, GSK, AstraZeneca, and the British Heart Foundation.
- Brain Health
Theme lead(s): Charlotte Warren-Gash
According to the National Institute on Aging, ‘brain health’ refers to how well a person’s brain functions across several areas. Aspects of brain health include:
- Cognitive health — how well you think, learn, and remember
- Motor function — how well you make and control movements, including balance
- Emotional function — how well you interpret and respond to emotions
- Tactile function — how well you feel and respond to sensations of touch, including pressure, pain, and temperature
Brain health can be affected by age-related changes in the brain, injuries such as stroke or traumatic brain injury, mood disorders such as depression, substance use disorder or addiction, and diseases such as Alzheimer’s disease.
The Brain Health Group investigates brain health in older age, including determinants of poor brain health, prevention strategies, care pathways and outcomes for people with conditions affecting brain health using a variety of large health datasets from different populations.
Some examples of our work include:
- A study showing a long-term increase in dementia risk after a range of common diagnosed infections, which was picked up by the Washington Post
- A study investigating whether infections affect cognitive decline or neuroimaging outcomes
- Studies of infections and cardiovascular outcomes including stroke
- Studies of inequalities in dementia diagnoses
We aim to improve scientific understanding of factors influencing brain health and, ultimately, to inform public health approaches to improving brain health in older age.
- Cancer
Cancer affects a huge number of people globally, and new treatments and prevention strategies are constantly being developed. Our research on cancer covers three main themes:
Long term health of cancer survivors
As the number of cancer-survivors increases, the long term health of these individuals is an increasing priority. The Beyond Cancer team, within the EHR Research Group, is examining the impact of cancer history and treatment on future risk of vascular diseases, mental health, quality of life, and other morbidities.
Medicines associated with cancer development
Research in this area aims to determine whether certain drugs have an impact on the risk of developing cancer. For example, our work has examined the impact of drugs such as angiotensin receptor blockers (used to lower blood pressure) on cancer, and PDE5 inhibitors on the risk of melanoma.
Cancer risk factors
Another strand of our work is to better characterise how potential risk factors for cancer are associated with specific cancers. A notable example was our work published in the lancet showing that BMI influences cancer risk in different ways for different cancer sites.
- Cardiometabolic Disease
Cardio-metabolic disease is an umbrella term, and in our group it covers the entities of diabetes and cardiovascular disease. Given that many people in the UK, and indeed globally, are affected by cardio-metabolic disease, this research theme is very important from a public health point of view. Our group uses electronic health records to answer questions relating to cardio-metabolic disease that ultimately help to improve our understanding of disease processes and disease outcomes. This is beneficial to patients, care providers, policy makers and the public at large.
- Infections / Vaccines / Immunity
Theme lead(s): Kate Mansfield, Ed Parker
Infectious diseases remain a major cause of ill health among individuals in the UK and elsewhere, particularly among the very young, among older individuals and among those with underlying health conditions. An increasing number of these diseases can be prevented by vaccination, and vaccination programmes are key public health tools for reducing illness due to infectious disease.
We use anonymised electronic health records to look at a wide range of important public health questions relating to infectious diseases – to monitor how common these conditions are, to identify risk factors for developing them, and to determine their outcomes. We are also assessing the effectiveness and safety of preventative measures such as vaccination. Separately, we are interested in other immune-mediated conditions, such as autoimmune diseases.
- Kidney Disease
Theme lead(s): Dorothea Nitsch
Our group is conducting a wide portfolio of research studies into aspects of kidney disease. We predominantly use Electronic Health Records and other sources of routine data. We are always interested in new collaborations and if you are interested in working with us please get in touch.
Kidney disease audits
The National CKD Audit ran until 2016 in England and Wales to provide a comprehensive picture of management and outcomes for people with chronic kidney disease (CKD) stages 3-5 in the region. It has now been replaced by CVDPREVENT (run by The Office for Health Improvement & Disparities), which audits a number of chronic conditions in primary care including CKD. Auditing CKD aims to improve the quality of patient care and assesses each GP practice against NICE CKD quality guidelines and standards to encourage quality improvement.
The UK Renal Registry (UKRR) is maintained by the UK Kidney Association. The UKRR audits the quality of care of people with advanced kidney disease including people. Dorothea Nitsch | LSHTM is currently the UKKA’s Director of Informatics Research.
General epidemiology of kidney disease
We are studying the impact of a range of risk factors and medications on the development and outcome of people with kidney disease using a number of routine data sources, including CPRD, and OpenSAFELY. During the COVID-19 pandemic we carried out a number of kidney-relevant analyses.
Global epidemiology of kidney disease
In addition to our research using EHRs we have a number of national and international collaborations investigating kidney disease in a global health context.
Links to some key publications:
- Defining measures of kidney function in observational studies using routine health care data: methodological and reporting considerations - PubMed (nih.gov)
- COVID-19 and kidney disease: insights from epidemiology to inform clinical practice - PubMed (nih.gov)
- Factors associated with COVID-19 vaccine uptake in people with kidney disease: an OpenSAFELY cohort study - PubMed (nih.gov)
- Comparative effectiveness of two- and three-dose COVID-19 vaccination schedules involving AZD1222 and BNT162b2 in people with kidney disease: a linked OpenSAFELY and UK Renal Registry cohort study - PubMed (nih.gov)
- Comparative effectiveness of sotrovimab and molnupiravir for preventing severe COVID-19 outcomes in patients on kidney replacement therapy: observational study using the OpenSAFELY-UKRR and SRR databases - PubMed (nih.gov)
- Identification of patients undergoing chronic kidney replacement therapy in primary and secondary care data: validation study based on OpenSAFELY and UK Renal Registry - PubMed (nih.gov)
- Sociodemographic features and mortality of individuals on haemodialysis treatment who test positive for SARS-CoV-2: A UK Renal Registry data analysis - PMC (nih.gov)
- Factors associated with COVID-19-related death using OpenSAFELY | Nature
- Association between practice coding of chronic kidney disease (CKD) in primary care and subsequent hospitalisations and death: a cohort analysis using national audit data - PubMed (nih.gov)
- A systematic review of statistical methodology used to evaluate progression of chronic kidney disease using electronic healthcare records - PubMed (nih.gov)
- Feasibility of evaluation of the natural history of kidney disease in the general population using electronic healthcare records - PubMed (nih.gov)
- How do primary care doctors in England and Wales code and manage people with chronic kidney disease? Results from the National Chronic Kidney Disease Audit - PubMed (nih.gov)
- The risk of acute kidney injury in colorectal cancer survivors: an english population-based matched cohort study - PubMed (nih.gov)
- Trimethoprim use for urinary tract infection and risk of adverse outcomes in older patients: cohort study - PubMed (nih.gov)
- Severe mental illness and chronic kidney disease: a cross-sectional study in the United Kingdom - PubMed (nih.gov)
- Stopping renin-angiotensin system blockers after acute kidney injury and risk of adverse outcomes: parallel population-based cohort studies in English and Swedish routine care - PubMed (nih.gov)
- Chronic kidney disease and cause-specific hospitalisation: a matched cohort study using primary and secondary care patient data - PubMed (nih.gov)
- Maternal Health
Theme lead(s): Caroline Minassian
The ability to conduct studies of maternal health using electronic health records depends crucially on identifying pregnancy episodes in the data source. While primary care records provide a rich source of maternity data, the precise timing of pregnancy can often be difficult to ascertain. To address this, we developed a new pregnancy identification algorithm in collaboration with researchers from the Clinical Practice Research Datalink (CPRD) to establish a Pregnancy Register in CPRD GOLD, and subsequently in CPRD Aurum. The GOLD and Aurum Pregnancy Registers list all pregnancies recorded within the corresponding primary care databases and include information on the start and end of pregnancy and the outcome (live birth, stillbirth, early pregnancy loss). The Registers are linked to CPRD primary care data and are available to researchers subject to protocol approval via CPRD's Research Data Governance Process.
We recently conducted further methodological work to investigate why the Pregnancy Register algorithm identifies some pregnancy episodes which are incomplete or conflicting (overlapping), and provide guidance on how best to handle these episodes in research studies.
Examples of work we have undertaken or are now initiating in the area of maternal health include:
- a study showing increased risk of pre-eclampsia following specific infections in pregnancy
- studies to investigate social factors associated with lower uptake of vaccines among pregnant women, and the safety of vaccines given in pregnancy
- studies of the effects of autoimmune diseases and their therapies on pregnancy outcomes
- a study investigating preconception management of hyperthyroidism and thyroid status in subsequent pregnancy
- Methodology
Theme lead(s): John Tazare
There are key methodological issues in the design and analysis of studies using routinely-collected data, including selection bias (e.g. minimising immortal time bias), missing data, measured/unmeasured confounding and the measurement of information being connected to underlying health status. Therefore, the use of complex statistical techniques is often required to ensure researchers obtain robust and valid conclusions from their analyses.
This group’s work aims to develop and evaluate such methodology (empirically and in controlled settings, e.g. using simulation studies) alongside providing practical guidance to support use of these techniques by applied researchers.
Our work coverages a range of methodological research topics, including:
- Benchmarking observational analysis against randomised controlled trials
- Innovative/novel study designs
- Case-crossover
- Clone-censor-weighting
- Prevalent new user designs
- Self-controlled case series
- Sequential trial designs
- Missing data methods
- Propensity score and disease risk score analysis
- Including extensions to high-dimensional propensity scores
- Quantitative bias analysis
- Risk prediction modelling
- Including issues surrounding their integration in electronic health record systems
- Simulating electronic health record data
- Target trial emulation
- Pharmacoepidemiology & Pharmacovigilance
Theme lead(s): Ian Douglas, Christopher Rentsch
The effects of medications are not completely known when a drug is first licensed for use by the general population. Important side effects might only become apparent when the drug has been used in very large numbers of patients, or for prolonged periods of time. Some effects might not have been seen because they happen more often in people who are unlikely to be included in randomised trials, such as people who take a lot of other medication, or who have several health conditions at the same time. The natural spread of age and gender are not always represented in trials, so information on drug effectiveness and side effects might be sparse for older age groups and, sometimes, women. Additionally, side effects of drugs such as heart attack and stroke are sometimes referred to as "rare" and the numbers of people in randomised trials are too small for these "rare" effects to be observed.
In pharmacoepidemiology, we study these effects in large groups of patients to give us a better idea of the overall balance of risks and benefits for a medication in the whole population. Not all effects are harmful; sometimes we might also be interested in finding out about the unintended benefits of a drug. Using primary care and linked electronic health records, we have been investigating these effects for many years. We have a strong interest in improving methodology for pharmacoepidemiology studies (see section on Methodology above), and work in a wide range of disease areas.
Some examples of our recent work include:
- Measuring utility of drugs thought to prevent or treat COVID-19 early in the pandemic, including hydroxychloroquine, inhaled corticosteroids, and anticoagulants
- Quantifying effectiveness of approved COVID-19 therapeutics
- A free, online textbook emphasising rigorous design and methodologies for real-world evidence aiming to inform clinical and regulatory decision-making during the pandemic
- Investigating the association between proton pump inhibitors and mortality and between fluoroquinolones and aortic aneurysm/dissection
- Using trial data to validate EHR analyses, with a COPD treatment example
Training
We offer annual training in pharmacoepidemiology, pharmacovigilance, and vaccine epidemiology, including:
- Professional Certificate in Pharmacoepidemiology & Pharmacovigilance
- Real-World Evidence in Pharmacoepidemiology
- Epidemiological Evaluation of Vaccines: Efficacy, Safety and Policy
For more details on these trainings, please visit the Training tab.
We also offer bespoke training programmes for organisations with specific requirements. If you may be interested in finding out more, please contact either Christopher Rentsch or Ian Douglas.
- Respiratory
Respiratory diseases are diseases that affect the airways, the bronchi and the lungs. They include acute infections, such as pneumonia and bronchitis, and chronic conditions such as asthma and chronic obstructive pulmonary disease.
Using large electronic databases, we study the long-term effects and outcomes of treatment for these chronic respiratory diseases. Asthma and COPD are very common illnesses, in which patients suffer from episodes of acute deteriorations of respiratory function termed exacerbations. There is increasing understanding that asthma and COPD are part of a spectrum of obstructive airway diseases consisting of complex subtypes which share certain characteristics (phenotypes) but differ in terms of prognosis.
Past work includes validation studies of COPD and acute COPD exacerbations in UK primary care electronic healthcare records and an ongoing validation study of asthma using the same data source. Other work focuses on the cardiovascular risk profile of COPD patients.
Currently, we are studying treatment patterns and control of different asthma phenotypes in the UK primary care electronic records.
Links to publications:
- The risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease: A systematic review and meta-analysis
- Predicting mortality after acute coronary syndromes in people with chronic obstructive pulmonary disease
- COPD disease severity and the risk of venous thromboembolic events: a matched case-control study
- Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study
- Skin Disease
Our research addresses an important research gap, the causes, consequences and treatment of skin disease. Little is known about the epidemiology of skin diseases. Our programme of works uses routinely-collected health data to provide answers to important research questions. These data include Electronic Health Records, Administrative data and Registry data.
Our work includes research on:
Herpes zoster - Examples include:
- Risk factors for herpes zoster
- Risk factors for post-herpetic neuralgia
- The role of zoster in triggering acute cardiovascular events
- Effectiveness of the zoster vaccine in routine use
We have well-developed national and international collaborations, involving colleagues in Canada the Netherlands, Denmark, and the USA. We are increasingly using data from different countries concurrently to answer the same research questions. We are always interested in new collaborations and if you are interested in working with us please get in touch. For further information on Dermato-Epidemiology, please see the European Dermato-Epidemiology Network.
Eczema – Examples include:
- Validating the diagnosis of eczema in UK general practice data (collaboration with colleagues at UPENN and UCSF)
- Long-term adverse outcomes with eczema
Other skin diseases - Examples include:
- Role of drugs in risk of malignant melanoma
We have well-developed national and international collaborations, involving colleagues in Canada the Netherlands, Denmark, and the USA. We are increasingly using data from different countries concurrently to answer the same research questions. We are always interested in new collaborations and if you are interested in working with us please get in touch.
For further information on Dermato-Epidemiology, please see the European Dermato-Epidemiology Network.
Amy
Mulick
Research Student - MPhil/PhD by Publication - Epidemiology & Population Health

Angel
Wong
Assistant Professor

Anne
Suffel
Research Fellow

Caroline
Minassian
Assistant Professor

Charlotte
Warren-Gash
Clin Prof of Epi & Health Data Science

Christopher T
Rentsch
Associate Professor

David
Lugo Palacios
Assistant Professor in Health Economics

Dorothea
Nitsch
Prof of Clinical Epide & HC Nephrologist

Edward
Parker
Assistant Professor

Elizabeth
Williamson
Prof of Biostats & Health Data Science

Emily
Herrett
Associate Professor

Georgia
Gore-Langton
Research Fellow

Helen
Strongman
Associate Professor

Helena
Carreira
Assistant Professor

Ian
Douglas
Professor of Pharmacoepidemiology

John Tazare
Research Degree Student

Julian
Matthewman
Research Fellow
Kirsty
Andresen
Research Student - MPhil/PhD - Epidemiology & Population Health

Krishnan
Bhaskaran
Professor of Statistical Epidemiology

Kwabena
Asare
Research Fellow

Laurie
Tomlinson
Professor of Clinical Epidemiology

Liam
Smeeth
Director

Louis
Tunnicliffe
Research Assistant

Luigi Palla
Assistant Professor

Patrick
Bidulka
Assistant Professor
Richard
Grieve
Professor of Health Economics Methodolog

Ruth
Costello
Research Fellow

Sinead
Langan
Professor of Clinical Epidemiology

Stephen
Evans
Emeritus Professor of Pharmacoepidemiology

Thomas
Cowling
Associate Professor
Ursodeoxycholic acid is a drug used to treat liver disease. It has been proposed that it may prevent severe COVID-19 outcomes, however previous studies of this have had inconsistent results.
What we did
We used electronic health records from people in England and identified people with two liver diseases: primary biliary cholangitis and primary sclerosing cholangitis. We looked at differences in COVID-19 hospitalisation and death between people taking UDCA and people who were not taking it.
Key findings
We found UDCA reduced the risk of severe COVID-19 outcomes by one-fifth. This suggests UDCA may help prevent serious COVID-19. Further clinical studies of UCDA should be undertaken, particularly in other groups with high risk or hospitalisation and death from COVID.
Citation: Costello RE, Waller KMJ, Smith R, Mells GF, Wong AYS, Schultze A, Mahalingasivam V, Herrett E, Zheng B, Lin LY, MacKenna B, Mehrkar A, Bacon SCJ, Goldacre B, Tomlinson LA, Tazare J*, Rentsch CT*, the OpenSAFELY Collaborative & the LH&W NCS (or CONVALESCENCE) Collaborative. Ursodeoxycholic acid and severe COVID-19 outcomes in a cohort study using the OpenSAFELY platform. Commun Med 4, 238 (2024). https://doi.org/10.1038/s43856-024-00664-y
What we did
We compared the impact of the pandemic using time-series analysis, in two countries that have similar, free at the point of use healthcare systems, but had different responses to the pandemic.
Key messages
We found that while there were already differences in cardiovascular hospitalisations by socioeconomic status, the pandemic did not significantly worsen these disparities overall, although there were some exceptions.
There were fewer admissions than expected during the pandemic for the most deprived quintile, compared to the least deprived quintile for:
- Heart failure in England
- Myocardial infarction in Denmark (though absolute numbers were smaller)
Conclusion
While it is positive that the pandemic has not worsened socioeconomic differences in cardiovascular admissions, further work is needed to understand the reasons for the differences seen.
Citation: Costello RE, Pedersen L, Henderson AD, et al. Impacts of the COVID-19 pandemic on deprivation-level differences in cardiovascular hospitalisations: a comparison of England and Denmark using the OpenSAFELY platform and National Registry Data. BMJ Open 2024;14:e088710. doi: 10.1136/bmjopen-2024-088710
Impact of NHS Data Opt-Outs on Health Research
In England, people can "opt out" of allowing their health data to be used for purposes beyond their direct care, like research or healthcare planning. In 2021, opt-outs rose sharply following government plans to create a centralized database of patient records, called the General Practice Data for Planning and Research (GPDPR). We aimed to understand how these opt-outs could impact health research.
Trends in Opt-outs
We found that between May 31 and June 30 2021 over 1.3 million people in England opted out, raising the total percentage of opt-outs from 2.77% to 4.97% of the population. This increase varied by sex, age, and region:
- By Sex: Among females, opt-out rates increased by 83%, from 3.02% to 5.53%. For males, the increase was 76%, from 2.51% to 4.41%.
- By Age: The largest increase was in people aged 40–49, where rates more than doubled from 2.89% to 6.04%.
- By Region: Opt-out rates varied across regions, but these differences did not clearly relate to local levels of deprivation.
Data are not available to assess opt-out trends by further characteristics.
Impact on Health Research
The substantial increase in opt-outs has important implications for health research in England, with two key issues:
- Sample size reductions: This can increase uncertainty and limit the ability to draw meaningful conclusions from the available data. With particular impact for the research of rare diseases and events.
- Distortion of findings: Systematic differences between people who opt-out and those who remain in the data have the potential to distort findings. It is not possible to detect or minimise these errors. This can lead to inappropriate policy decisions based on these findings.
Conclusion
The rise in opt-out rates was not uniform across all groups and regions, and its full impact on health research is hard to measure. Importantly, it is not possible to quantify or mitigate this impact adequately using data available to researchers. The study highlights the need for careful consideration of the potential effects of opt-outs on research and health policies when creating future national data-sharing initiatives.
Citation: NHS national data opt-outs: trends and potential consequences for health data research. John Tazare, Alasdair D Henderson, Jessica Morley, Helen A Blake, Helen I McDonald, Elizabeth J Williamson, Helen Strongman. BJGP Open 9 July 2024; BJGPO.2024.0020. DOI: 10.3399/BJGPO.2024.0020
New research conducted by the Beyond Cancer team at LSHTM has demonstrated an increased risk of broken bones among cancer survivors. This study, funded by the Wellcome Trust and published in Lancet Health Longevity, analysed electronic health records from over 578,000 cancer survivors and 3.2 million cancer-free individuals, revealing important insights into bone health after cancer diagnosis.
The authors found that compared to those without cancer, cancer survivors are at a heightened risk of bone fractures overall, as well as fractures associated with osteoporosis – a health condition that causes weakened bones.
The risks varied across different types of cancer, with multiple myeloma and prostate cancer survivors particularly affected. While the heightened risk of fractures tended to be most pronounced shortly after cancer diagnosis, risks remained elevated to some extent for more than five years in several cancer types, underscoring the importance of ongoing monitoring and preventive measures.
Study co-lead Helena Carreira said: “These findings emphasize the need for increased awareness and management of bone health among cancer survivors. Healthcare providers should consider implementing long-term monitoring strategies and tailored preventive measures to reduce the risk of fractures in this population.”
This study underscores the importance of bone health in cancer survivorship care and highlights the need for continued research and support for individuals navigating life after cancer.
Citation
Buzasi E, Carreira H, Funston G, Mansfield KE, Forbes H, Strongman H, Bhaskaran K. Risk of fractures in half a million survivors of 20 cancers: a population-based matched cohort study using linked English electronic health records. The Lancet Healthy Longevity 2024. doi: 10.1016/S2666-7568(23)00285-4 PMID: 38335985
A recently published paper sheds light on the disparities in the management and outcomes of acute myocardial infarction (AMI) in patients with kidney impairment in England. The study, which used linked data from four national healthcare datasets, investigated how people’s kidney function (measured using the estimated glomerular filtration rate (eGFR)) affected their AMI care between 2015 and 2017.
AMI is a major health concern that leads to significant mortality and morbidity, particularly in individuals with impaired kidney function. Previous research in the United States of America has indicated disparities in care, but this study aimed to determine whether similar findings extended to Europe and the UK.
The research, led by Patrick Bidulka (Research Fellow - LSHTM), Jemima Scott (NIHR Doctoral Clinical Research Fellow - University of Bristol), David Adlam (Professor - University of Leicester), and Dorothea Nitsch (Professor - LSHTM) found several clinically important results in their analysis:
Reduced Odds of Invasive Management: The study examined a cohort of 5,835 individuals and found that people with eGFR levels less than 60 mL/min/1.73m² (indicating kidney impairment) were less likely to receive invasive management compared to those with eGFR levels equal to or greater than 60 when hospitalized for non-ST segment elevation MI (NSTEMI).
Variation in Management for STEMI Patients: The association between eGFR levels and the odds of invasive management for ST-elevation MI (STEMI) varied depending on the availability of percutaneous coronary intervention (PCI), also known as angioplasty. However, where PCI services were available all the time, almost all people with STEMI received PCI no matter their baseline kidney function.
Graded Association with Mortality: The study demonstrated an association between worsening baseline eGFR stage and increasing risk of mortality after adjusting for several confounders, both in-hospital and after discharge.
These findings highlight significant disparities in the care and outcomes of AMI patients in England based on their baseline eGFR levels measured in primary care. Encouragingly, the study suggests that these disparities may be decreasing over time, with the least difference seen in patients with STEMI who are managed through the primary percutaneous coronary intervention pathway.
These insights have important implications for healthcare professionals and policymakers, emphasizing the need for tailored care strategies for AMI patients with kidney impairment. Reducing disparities in care and improving outcomes for this vulnerable population should be a priority.
This paper is the second paper published by this team – the first paper looked at differential AMI case ascertainment by eGFR stage across secondary care datasets commonly used in epidemiological research in England.
These studies underscore the need for continued efforts to understand the drivers of AMI treatment disparities and outcomes for people with kidney impairment to ultimately improve the health of this vulnerable population.
Patrick Bidulka, the joint-lead author of this paper, is pleased to have completed this study. He is now building on these findings to investigate the comparative effectiveness of invasive versus conservative AMI treatment among people with kidney impairment, using the natural variation in AMI processes of care in similarly linked national health data sources.
The authors would like to thank the funders of this research: Kidney Research UK and The Health Foundation.
Citation:
Scott J, Bidulka P, Taylor DM, Udayaraj U, Caskey FJ, Birnie K, Deanfield J, de Belder M, Denaxas S, Weston C, Adlam D, Nitsch D. Management and outcomes of myocardial infarction in people with impaired kidney function in England. BMC Nephrol. 2023 Nov 2;24(1):325. doi: 10.1186/s12882-023-03377-x. PMID: 37919679; PMCID: PMC10623815.
We wanted to understand if using certain antibiotics called fluoroquinolones increases the risk of aortic aneurysms or dissections, which are serious heart problems. Earlier studies showed a connection, but it wasn’t clear if it was causal.
We did two kinds of studies using electronic medical records from the UK. In a cohort study, we followed a group of people over time to see if those who took fluoroquinolones were more likely to be hospitalised with the heart issues than people taking other types of antibiotic. In a case crossover study we looked at people with the heart problems to see if they were more likely to have been prescribed a fluoroquinoloine shortly before the heart problem compared with other times in their history when they didn’t have a heart problem.
In both designs we found that fluoroquinolone use was associated with aortic aneurysm, but that after accounting for confounding, there was no difference in the risk with fluoroquinolones compared with alternative antibiotics. This suggests earlier studies may have over estimated the risks with fluoroquinolones and we believe these findings should help doctors make choices when treating infections with antibiotics.
Study Authors:
Jeremy P. Brown, MSc; Kevin Wing, PhD; Clémence Leyrat, PhD; Stephen J. Evans, PhD; Kathryn E. Mansfield, MBBS, PhD; Angel Y. S. Wong, PhD; Liam Smeeth, MBChB, PhD; Nicholas W. Galwey, PhD; Ian J. Douglas, PhD
Available at:
JAMA Cardiol. 2023; 8(9):865-870. doi:10.1001/jamacardio.2023.2418
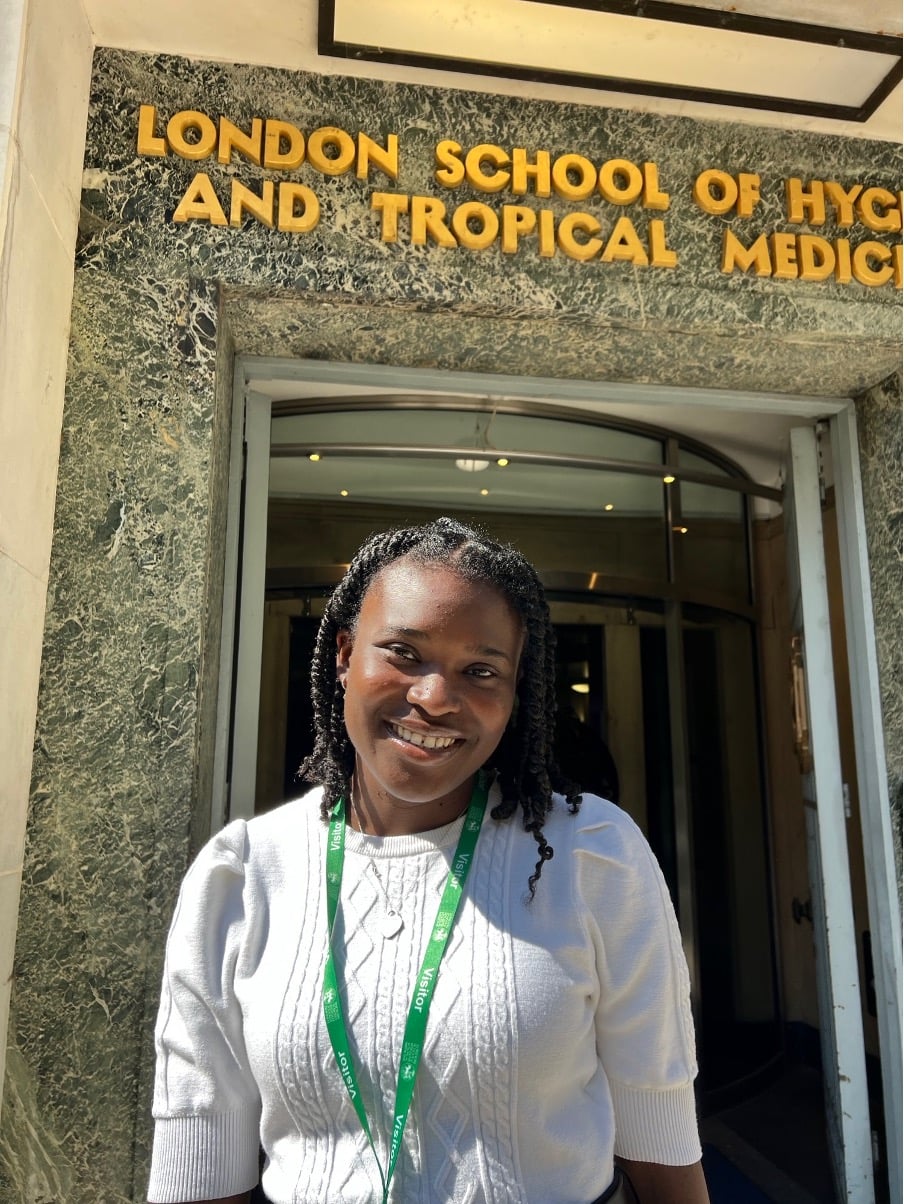
My elective at the London School of Hygiene and Tropical Medicine this summer built on my clinical foundations and prior research experience to provide unique new insight into the field of Academic Dermatology. My interest in social determinants of health was sparked whilst completing my MSc in Global Health, where I was introduced to the social impacts of dermatological conditions. Although medical school provided me with an essential understanding of eczema diagnosis and treatment, this elective facilitated engagement with exciting research already in the pipeline, alongside novel artistic endeavours focusing on public engagement.
Systematic review
My time at LSHTM built on experience from my intercalated MSc to cultivate vital skills for clinical research. During meetings with my supervisor and other collaborators from international institutions, we discussed the beginnings of a systematic review to explore associations between allergic diseases, such as eczema, and their relation to educational attainment and occupational status. This provided me with the basis to begin reviewing literature, including research suggesting that allergic diseases in childhood may hinder ability to attain educational achievements and occupational status. Literature highlights that eczema, asthma and allergy are closely associated with impaired dietary intake, school absence, and stigma. My understanding of this topic and the required systematic review processes were consolidated through the Systematic Review and Meta-Analysis course from Johns Hopkins University, for which I gained a certificate of completion. These opportunities have provided me with the foundational knowledge to contribute towards a systematic review, leading on from this elective.
Research group meetings
Being based with the Faculty of Epidemiology and Public Health provided the oppourtunity to attend meetings with the Electronic Health Records Research Group, as well as the Skin Disease Epidemiology and Health Data Research Group. This provided practical techniques for making research clinically relevant, as well as opportunities to learn from leading clinicians in Academic Medicine. Meetings were enriched by staff and students from a diverse variety of disciplines, each contributing to collaborative discussions, including the EHR journal club and Primary Health Care Infrastructure webinar. There were also opportunities to learn from experts in the field, including a seminar led by Professor David Margolis exploring antibiotic use in skin disease. Attending research meetings taught me how health data records can vary in both quality and accessibility between countries, as well as the benefits and challenges of using electronic health records. The process of critically appraising generalisability for patient demographics of interest has also been an essential learning point for me, as this will be key for my future delivery of evidence-based medicine using a patient-centred approach.
Creativity and collaboration
In a unique opportunity to collaborate with creators of the ‘Colouring Adult Eczema’ exhibition, I produced an article detailing updates and feedback from their nationwide tour. For patients living with eczema, complex interactions between health determinants results in heterogeneous lived experiences, which have been recently explored through use of artistic workshops and sculptures. I am inspired by the wonderful work from this collaborative team of artists and researchers, which will help to address the health and social inequalities for patients living with eczema.
Final reflections
My experience during my medical elective at LSHTM has shown me the highly collaborative nature of clinical research, whilst cultivating fundamental skills required for the field. Following this, I feel better equipped to enter my Specialised Foundation Programme Training with the aspiration and practical tools for pursuing a career in Academic Dermatology. I would like to thank my supervisor Professor Sinéad Langan and the Skin Disease Epidemiology and Health Data Research Group, alongside the wider Electronic Health Records Research Group, for welcoming and supporting me throughout the elective.
Background: Jemima has just completed her medical degree from Brighton & Sussex Medical School. In 2021 she completed her intercalated MSc in Global Health at Maastricht University in the Netherlands and a Global Burden of Disease elective at McMaster University in Canada.
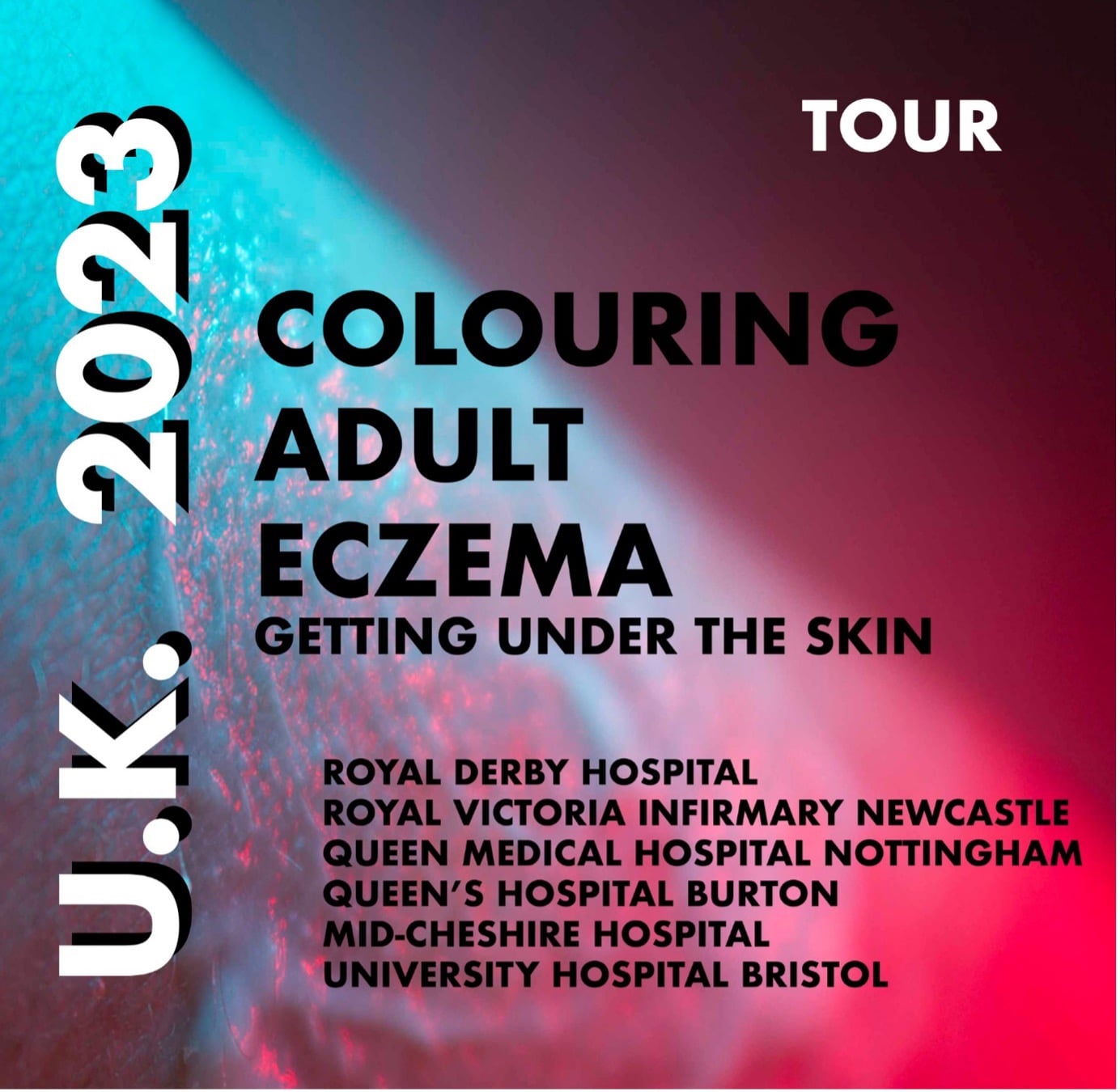
Since 2019, the ‘Colouring Adult Eczema’ art project has intrigued and inspired the public, using creative storytelling to explore the experiences of adults living with eczema. This unique utilisation the Arts for public engagement offers new insight on the impacts of the condition. Now on a nationwide tour, the project continues to resonate with individuals from a variety of locations and backgrounds.
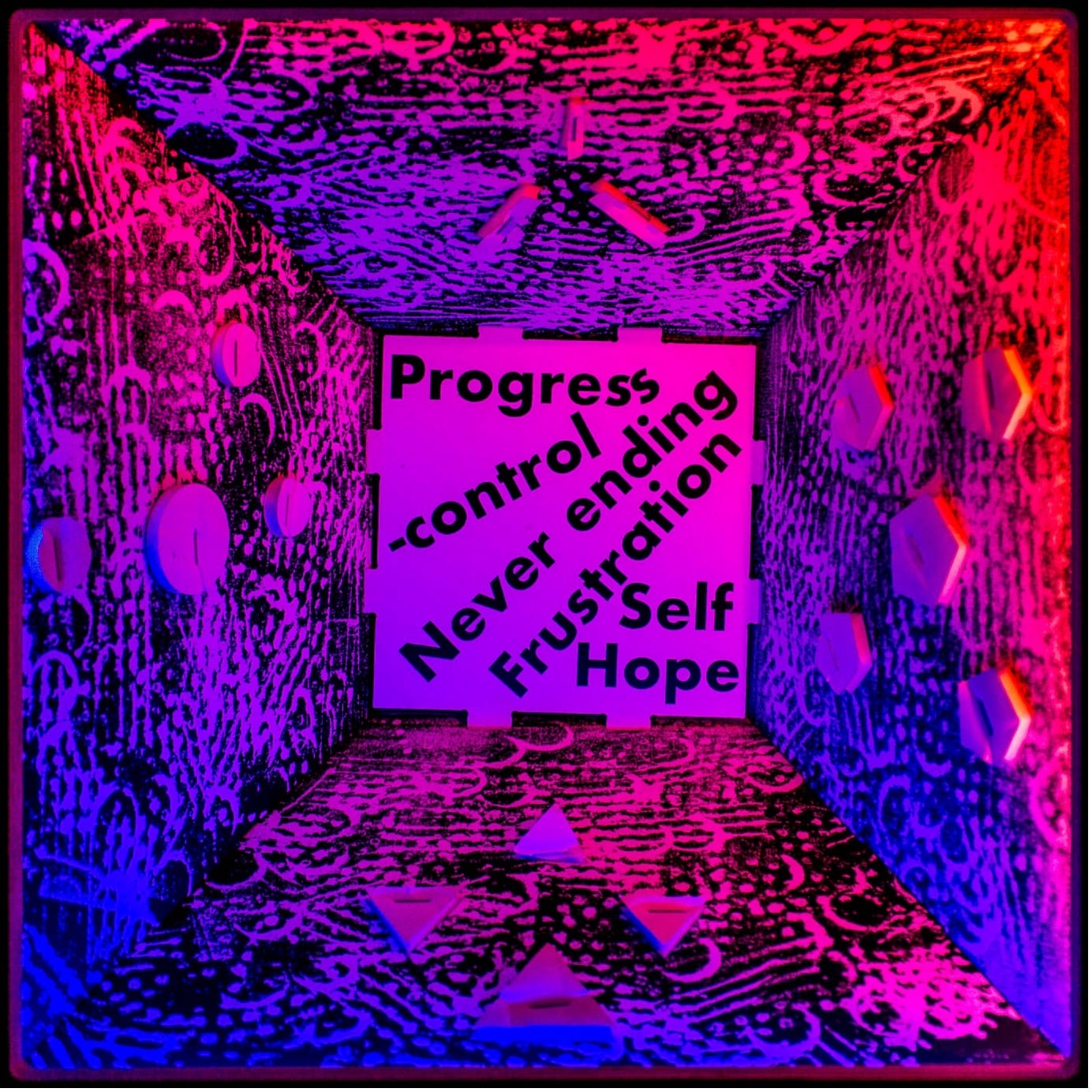
The project was commissioned by Professor Sinéad Langan at the London School of Hygiene & Tropical Medicine, with support from the Wellcome Trust. Lead Artists Peter Hudson and Julia Vogl first conducted workshops in Summer 2019, in collaboration with 30 adults living with eczema across the UK. Workshop participants shared their unique lived experiences using a variety of sensory modalities, including poetry and printmaking. These resources were used by Vogl and Hudson to design and create bespoke LED boxes, which were artistically combined to produce a sculpture.
LONDON
Following the sculpture’s world premiere at the 2022 British Association of Dermatology Conference in Glasgow, the exhibition went on to have its debut at Guy’s Hospital in London during National Eczema Week in 2022 and is currently on tour across the UK.
Each of the boxes encapsulated within the sculpture details an individual experience – each one uniquely different from the surrounding boxes. These represent experiences that extend beyond the unifying diagnosis of eczema and its well-known physical symptoms, including itch and discomfort. The project offers deeper reflection on the psychosocial impacts of the condition, including personal relationships and mental health. Hence, this public engagement art project demonstrates the increasing need to advocate for adults living with eczema, due to the longitudinal health and social impacts of the condition.
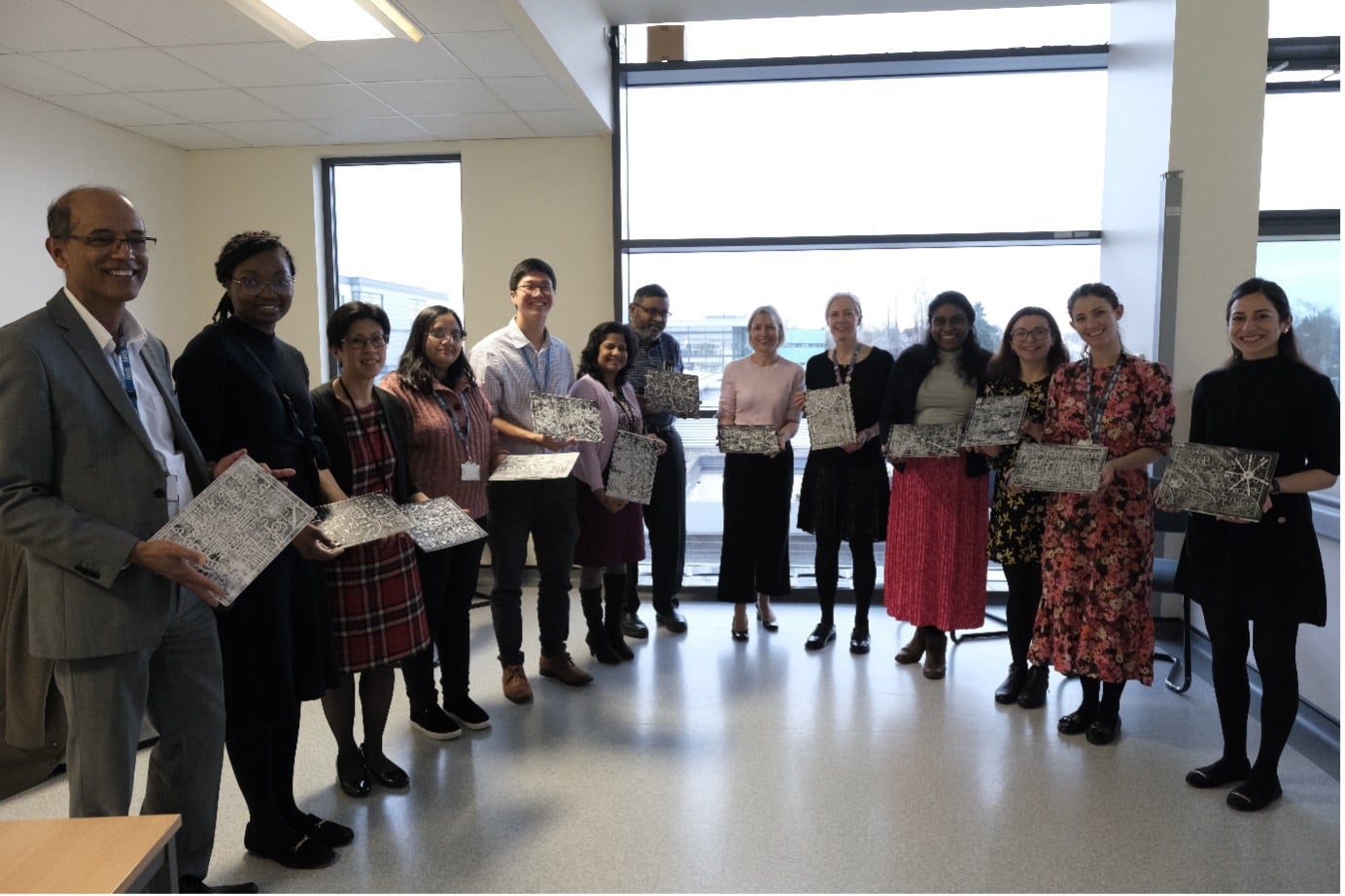
DERBY
The above image shows staff members in Derby, who participated in a workshop with the artists whilst the sculpture was at their site. Similar workshops have taken place at each site to enhance understanding of how the sculpture was made and facilitate connections around eczema.
NEWCASTLE
The exhibition facilitated a depth of reflection that was also displayed through the richness of participant feedback. Following a recent display at the Royal Victoria Infirmary in Newcastle, participants expressed their regard for the “lovely, thoughtful” nature of the exhibit, which allowed them to “share with people”. Other participants appreciated the exhibition’s visual appeal, conveying how they “love the colours”.
Visibility for the frequently unseen impacts of eczema was a common theme, with one participant expressing "it's good to see something aimed at improving the public's awareness of eczema and understanding of the condition”. This participant reflected further on the “beauty of the artwork [which] contrasts with the message that reflects the reality of those living with eczema". This juxtaposition of beauty and difficulty is integral to the exhibition’s design, as expressed by Peter Hudson, one of the project’s Lead Artists:
“There’s been a real need for adults to share their stories and experiences of living with eczema, and it’s been a real honour to share a platform and artwork for communicating it to a wider audience. The fact that the condition is so widely misunderstood is partly a cause of the inevitable shame people with eczema can end up feeling about it. Anything that helps people understand eczema better is a good thing. I hope that the contrast the sculpture creates between being bright and colourful in appearance, yet emotional, intimate and dark at times in subject matter, helps to almost catch people off-guard, so they engage with the piece more deeply”
-Peter Hudson
The aesthetically driven social media platform Instagram has also increased accessibility to the exhibition and facilitated further engagement with the public. One Instagram user commented on their personal experience, "…as a sufferer of severe atopic eczema, I believe it is important to share how much it actually affects people. I have tried sharing knowledge to others through poetry which I hope will make a difference like this project”. As one of the Lead Artists for the exhibition, Julia Vogl discussed the intentional complexity of the sculpture’s design in advocating for adults living with eczema:
“Eczema means different things for different people, but in my involvement in this project since 2019, I have learned that there is a communal wish to share. That many with eczema want greater compassion in society so that the coping mechanisms - weather it be diet, clothing, where they holiday, and even what job they do- is not judged but met with empathy. So much of living with eczema in adulthood is beyond the itch - it determines lifestyle. This sculpture touring across the country is meant to broaden empathy and empower those with the condition, they are not alone.”
-Julia Vogl
FINAL THOUGHTS
Despite being visible on a person’s skin, the psychosocial impacts of eczema have remained largely unseen until recently. The ‘Colouring Adult Eczema’ art project is providing a safe space for members of the public to learn and share about the impacts of eczema, as well as reflecting on their own lived experiences. The increasingly hybrid nature of modern life is being well-utilised throughout the tour, combining the beauty of in-person exhibitions with a growing online community that connects individuals with shared interests. The insight gained from the project will contribute towards identifying and holistically addressing the biological, psychological and social impacts of eczema, aiming to maximise the quality of life for those living with the condition.
The exhibition is still available to experience on tour during the following dates at their corresponding locations:
- May 24th to June 27th: Nottingham – Nottingham NHS Treatment Centre, Queen’s Medical Centre, Nottingham University Hospitals NHS Trust
- June 28th to August 1st: Burton – Queen's Hospital Burton, University Hospitals Derby and Burton NHS Foundation Trust
- August 2nd to September 12th: Mid Cheshire – Mid Cheshire Hospital, NHS Foundation Trust
- September 12th to October 25th: Bristol – UHBW Arts & Culture, University Hospitals Bristol and Weston NHS Foundation Trust
New dates have been added for Mid Cheshire and Bristol as part of Eczema awareness week, which officially marks a one year journey for the sculpture.
To keep up to date with the progress and feedback about the project, visit the Instagram page at @colouringadulteczema. To read more about the ‘Colouring Adult Eczema: Getting Under the Skin’ exhibition, visit the article Colouring Adult Eczema: Getting Under the Skin | Stories of engagement | LSHTM
During the Summer of 2021, I undertook a jampacked, six-week internship at the London School of Hygiene and Tropical Medicine (LSHTM) in collaboration with Health Data Research (HDR) UK. The internship was organised as part of the 10,000 Black Interns Programme. I applied because I wanted to understand what happens ‘behind the scenes’ when healthcare professionals see patients, i.e., what happens to their data and how this is applicable to research. I specifically applied to LSHTM because of its track-record in global health research, a subject I am deeply passionate about.
Each week of the internship offered a new opportunity to learn more skills and meet new people whether that be other interns at partner institutions, academics, and industry professionals. Within the first week, I had received training in data protection, the Clinical Practice Research Datalink, a briefing from my project supervisor and I was ready to go. In the second week, I attended the UCL Institute of Health Informatics’ work experience initiative where I was exposed to research ethics and governance, record linkage and bias in health data research.
My project was on the COVID-19 Outbreak Investigations to Understand Transmission Study (COVID-OUT). COVID-OUT falls under Theme 1 of the PROTECT COVID-19 National Core Study on Transmission and Environment. The aim of the study is to understand SARS-CoV-2 transmission routes and risk factors through investigation of outbreaks in a range of occupational settings. During my time at the School, I participated in the analysis and preparation of the outbreak investigation reports.
The project is co-opted by LSHTM, the Health and Safety Executive, Public Health England, and the University of Manchester. Therefore, through joining this project, I oversaw how epidemiological teams worked together and gained experience in outbreak investigations, which apply to all healthcare contexts. This has motivated me to continue to get involved with work at this scale in future. A highlight of the 6 weeks, working on this project, was the opportunity to co-present with my supervisor, Dr Elizabeth Brickley, at the International Festival of Public Health. It was a unique chance for me to improve my presentation skills and public speaking. I am grateful for my supervisor’s encouragements and ‘can-do’ attitude all throughout.
A running theme throughout the internship was of scholarship. I joined the LSHTM Health Equity Action Lab’s biweekly journal club focusing on decolonising global health. I attended panel talks and one-to-one sessions with both senior and junior academics and gleaned advice from both ends of the spectrum. Alongside this, I attended a series of careers workshops and even spoke with Senior Careers Consultant Penny Longman about pathways into careers in global health as a medic.
With 8 co-interns at other partner institutions, we undertook the HDR UK Technical Team Challenge. We worked well as a team, building on our strengths and weaknesses in skills like report writing, data profiling and data visualisation. Our strategy worked as we came 1st place out of all the teams. HDR UK also organised ‘Friday Takeovers’ where we interacted with representatives from academic and charitable institutions that are using data science to improve the lives of patients.
Through this internship I have gained a broadened understanding of health data science and contributing factors to COVID-19 outbreaks in the workplace, a network of like-minded people and increased confidence in my abilities. I would really encourage prospective applicants to apply and be open to projects and discussions you may not have encountered.
I would like to thank Prof Sinéad Langan, Prof Elizabeth Williamson, Paris Baptiste, and Jack Whitelegg from LSHTM for organising and supporting us throughout this internship. Thank you to my supervisors Dr Elizabeth Brickley, Dr Amber Raja and the team at COVID-OUT. I would also like to say a massive thank you to Tammy Palmer, partners at Health Data Research UK and to the 10,000 Black Interns Campaign. This has been a truly life-changing experience and I hope this kind of internship continues at the School.
Adanna Ewuzie is a medical student at Queen’s University Belfast who will be taking a year out in 2021/22 to study an MSc in Global Health Science and Epidemiology at the University of Oxford.
For the last 6 weeks, I have had the opportunity to be part of the Black Internship Program that was organized by Health Data Research (HDR) UK and hosted by several partner organizations including my host - the London School of Hygiene and Tropical Medicine (LSHTM).
My experience during this internship was extremely exciting, insightful, and far beyond what I had expected. At LSHTM I had the opportunity to work on a survival analysis project that was investigating the impact of frailty on early hospital readmission, heart failure, stroke, and mortality after an acute kidney injury (AKI) discharge. This project expanded my data analysis skills and code writing in both Stata and R as well as data presentation. I received well thought out guidance from the project coordinators (Laurie Tomlinson, Patrick Bidulka and Paris Baptiste).
The other very inspiring project that I worked on was a technical team challenge organized by HDR UK. This was group work led by a team of nine interns from different host institutions. The machine learning project involved looking at the predictors of Mental Health illness and treatment. This was my first time working on a machine learning project in Python and it provided a massive leap in my Python programming skills.
The icing on the cake during this internship was the opportunity to learn from people with different career backgrounds and their work in Health Data Science. The interactions during this period were very intuitive and gave me a new perspective on the available opportunities in Health Data Science. I especially appreciated work experience with colleagues at UCL and panel talks with several professionals in various stages of their career. The panel talks provided wise counsel that will be helpful in my career.
The other good part of this internship is that it offered several opportunities for mentorship and collaboration.
Last but not least, the support from my host, LSHTM was amazing. The entire team, led by Sinead Langan and Elizabeth Williamson and assisted by Jack Whitelegg and Paris Baptiste did a wonderful job to ensure we had the best experience!
Finally, I would like to appreciate my HDR UK mentor Caroline Cake, the CEO of HDR UK, Tammy Palmer and HDR UK for organizing this internship program.
Study findings suggest that this group will also have a greater chance of severe COVID-19 outcomes
There are nearly 2 million cancer survivors in England. Although, people under current treatment for cancer were recognised early on as being a high-risk group for severe COVID-19, it was unclear whether this much larger population of medium- to long-term cancer survivors might be considered vulnerable to severe disease. Researchers in the Beyond Cancer Team, part of the LSHTM Electronic Health Records Group, addressed this by looking at historical data on another similar epidemic respiratory virus, influenza.
The researchers compared the risk of influenza hospitalisation or death between cancer survivors and cancer free controls. The study included data from 108,215 cancer survivors and 523,641 people with no prior cancer. Survivors of blood cancers had substantially elevated risks of influenza hospitalisation or death persisting for at least 10 years after cancer diagnosis, while risk was doubled for survivors of other cancers for up to 5 years from diagnosis. Cancer survivors were also more likely to have other illnesses that have been associated with higher risk of severe COVID-19 disease, such as diabetes and heart disease.
Flu vaccination has been historically recommended for people with some active cancers or with current or recent cancer treatment. The results of this study suggest that a wider population of longer-term cancer survivors might need to be prioritised for vaccination against both influenza and COVID-19.
Read the full paper on EClinicalMedicine.
Lead authors Helena Carreira and Helen Strongman can be reach by email at helena.carreira@lshtm.ac.uk and helen.strongman@lshtm.ac.uk
Check also the Beyond Cancer website, and stay up-to-date with our news on Twitter @beyondcancer0
Nationwide observational study on pre-exposure use of hydroxychloroquine could help recruitment into ongoing clinical trials
Early in the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic, it was suggested that hydroxychloroquine - a commonly used treatment for rheumatic diseases - might have benefits for the treatment and prevention of COVID-19. Hydroxychloroquine has since been investigated in several randomised clinical trials and observational studies. Most studies to date have shown no evidence of a benefit of hydroxychloroquine as a treatment for patients admitted to hospital who already have COVID-19.
A separate question remains: does routine ongoing use of hydroxychloroquine in people without coronavirus infection protect against new infections or severe COVID-19 outcomes? We studied a large number of people who were prescribed hydroxychloroquine as part of normal clinical care and followed them up to look for signals of benefit or harm in mortality from COVID-19 and other causes. We found no evidence of benefit or harm after adjusting for important differences between people with the same health conditions who were prescribed hydroxychloroquine or not.
The scientific community should endeavour to encourage recruitment to trials like COPCOV since, in the absence of a vaccine, there are no current preventative treatments available. This paper adds to evidence of scientific equipoise and can help with recruitment. The use of hydroxychloroquine for prevention of COVID-19 mortality outside trial settings is currently not justified.
Read the full paper on The Lancet Rheumatology.
Commentary on the piece can be found on the Lancet and LSHTM sites.
Lead author Christopher Rentsch can be reached by email at christopher.rentsch@lshtm.ac.uk or on Twitter @DarthCTR
Tune into the King’s Fund Digital Health and Care Conference, where our very own Rohini Mathur and Liam Smeeth, along with Ben Goldacre and Caroline Morton of the Oxford DataLab, and Chris Bates from the GP software company TPP discuss the development of OpenSAFELY – a data analytics platform, built to deliver large-scale COVID-19 research in just 42 days.
In this roundtable session, they will discuss the technical aspects of creating OpenSAFELY, the philosophy of open and collaborative working underpinning the platform, and early findings from their studies.
Full conference runs 2-5 November 2020. The team's session is 3 November 11am-12pm GMT (Session 5).
Link to sign up: https://www.kingsfund.org.uk/events/digital-health-and-care
New estimates suggest strategies to reduce the risk of cardiovascular disease are needed for the growing population of cancer survivors
Survivors from a wide range of cancers could experience increased risks of heart disease and blood circulation problems compared to those who have never had cancer, according to new estimates published in the Lancet.
In one of the largest studies of its kind, the research team, led by members of the EHR Research Group at the London School of Hygiene & Tropical Medicine, analysed the medical records of more than 630,000 people in the UK, including over 100,000 survivors of a range of cancers.
They found raised risks of blood clots forming in the veins among survivors of most cancers, ranging from approximately a two- to ten-fold increase in risk for different cancer sites. Risks decreased over time but were still elevated for more than five years after the cancer diagnosis. Survivors of half of the 20 cancers studied also faced increased risks of heart muscle damage, known as cardiomyopathy, and heart failure.
For example, survivors of blood, oesophagus, lung, kidney and ovarian cancers were more than one and a half times more likely to experience cardiomyopathy or heart failure than people with no prior cancer.
An increased risk of coronary artery disease and stroke was found in some cancer survivors, including those with prior blood cancers.
The researchers stress that for many people the overall risks will still be low, particularly for younger cancer survivors, but say the findings highlight the need for new strategies to prevent and manage heart and circulation problems in cancer survivors, including a need to raise awareness among GPs of the raised risks.
While the researchers could not definitively identify the causes of the increased risks, the team’s analysis suggests that exposure to cancer treatments such as chemotherapy is likely to play a key role.
Lead author Helen Strongman from the London School of Hygiene & Tropical Medicine said: “Over recent decades cancer treatment and management have improved substantially, resulting in a large and growing population of long-term cancer survivors. Around half of those diagnosed with cancer in developed countries are now expected to survive for more than 10 years. However, there are concerns that there may be increased long-term risks of cardiovascular disease following cancer diagnosis, driven by treatment side-effect effects and the potential impact of the cancer itself.”
While previous studies have demonstrated the short- to medium-term increased risk of cardiovascular disease from some specific cancer treatments, there have been limited data on the overall and long-term differences in cardiovascular risk between cancer survivors and those who have never had cancer.
To address this, the team brought together anonymised data from primary care, hospitals, cancer registries, and death certificates, to quantify the absolute and relative risks of a comprehensive range of cardiovascular diseases in survivors of the 20 most common adult cancers1, compared with cancer-free general population controls. The research also accounted for other risk factors for cardiovascular disease, such as older age, smoking and body mass index.
The team found large increases in risk of venous thromboembolism (blood clots in the veins) among survivors of 18 of the 20 cancers studied compared to cancer-free controls. Survivors of breast cancer had double the risk of venous blood clots one year after diagnosis compared with similar women with no prior cancer, though the overall level of risk remained low, especially for younger survivors.
For female breast cancer survivors aged under 60 years, six extra blood clot cases per year were observed per 1,000 women, while among older women (80+ years) 12 extra cases per year were observed per 1,000 women. These risks decreased over time but remained elevated for at least five years after diagnosis with most cancers.
The team also observed long-term increased risks of heart failure and heart muscle damage among survivors of 10 of the 20 site-specific cancers studied. Among people who had non-Hodgkin lymphoma five years previously, there were four extra cases of heart failure per year for every 1,000 people aged under 60, rising to 21 extra cases per year for every 1000 people aged over 80 years.
The senior author of the study Professor Krishnan Bhaskaran from the London School of Hygiene & Tropical Medicine said: “With treatment for cancer becoming more effective, we must start thinking about living beyond cancer and improving the health of survivors. Our work revealed raised risks of various cardiovascular diseases in cancer survivors. These findings are important because those affected might benefit from preventative measures and earlier interventions to reduce the impact.
"If patients, primary care doctors, and specialists are more aware of the potential for increased cardiovascular risks in this patient group, we might detect problems earlier and improve outcomes. There is limited guidance at present to help doctors manage cardiovascular risk in cancer survivorship, and further evidence is needed on whether routine monitoring or additional preventative measures would benefit those with the highest risks."
The authors acknowledge limitations of their study including that there was only limited information available about the anti-cancer treatments that patients had received. Although the research team had some information on whether patients had received chemotherapy, radiotherapy, and surgery, there was no detailed information on specific chemotherapy drugs, radiotherapy doses, or surgery procedures.
The study was funded by the Wellcome Trust and the Royal Society.
Publication
Helen Strongman, Sarah Gadd, Anthony Matthews, Kathryn E Mansfield, Susannah Stanway, Alexander R Lyon, Isabel dos-Santos-Silva, Liam Smeeth, Krishnan Bhaskaran. Medium and long-term risks of specific cardiovascular diseases in survivors of 20 adult cancers: a population-based cohort study using multiple linked UK electronic health records databases. The Lancet. DOI: 10.1016/S0140-6736(19)31674-5
The Electronic Health Records (EHR) Research Group at the London School of Hygiene & Tropical Medicine are pleased to announce they are now accepting applications for two longstanding pharmacoepidemiology and pharmacovigilance short courses: Professional Certificate in Pharmacoepidemiology & Pharmacovigilance and Practical Pharmacoepidemiology. Details about this year’s courses are provided below.
Accreditation: Both face-to-face courses have been approved by the Federation of the Royal Colleges of Physicians of the United Kingdom for Category 1 (external) Continuing Professional Development (CPD) credits (Professional Certificate in Pharmacoepidemiology & Pharmacovigilance = 30 credits; Practical Pharmacoepidemiology = 20 credits).
Professional Certificate in Pharmacoepidemiology & Pharmacovigilance
Course dates: 4 – 7 November 2019, 17 – 21 February 2020, 6 – 9 April 2020 (also available via distance learning)
This course is a 30-week examined introductory training course that aims to equip students with a basic understanding of the concepts and practice of pharmacoepidemiology, pharmacovigilance and drug safety. By the end of the course, students will be able to:
- Demonstrate an understanding of, and critically evaluate, issues surrounding the risks and benefits of drug use in humans
- Gain an understanding of, and reflect upon, important pharmacoepidemiological concepts and methods
- Assess and critically analyse the results of pharmacoepidemiological studies (other investigators'), including critical appraisal of the study question, study design, methods and conduct, statistical analyses and interpretation
Find out more about the Professional Certificate in Pharmacoepidemiology & Pharmacovigilance course. Anyone with questions about the course content/suitability can contact Dr. Kevin Wing or Dr. Rohini Mathur at Kevin.Wing@lshtm.ac.uk or Rohini.Mathur@lshtm.ac.uk.
Practical Pharmacoepidemiology
Course dates: 16 – 19 September 2019
The course is designed for students with a basic grounding in epidemiological methods and concepts and/or some prior knowledge of pharmacoepidemiology (which could include people who have already completed the Professional Certificate in Pharmacoepidemiology & Pharmacovigilance at LSHTM). During this course students will:
- Develop their knowledge of pharmacoepidemiological concepts and methods, with a particular focus on database studies.
- Gain practical experience of testing study feasibility and performing analyses in STATA, using primary care data from the Clinical Practice Research Datalink (CPRD) (prior experience of STATA not required).
- Gain an understanding of biases and other sources of error that can occur in pharmacoepidemiology studies, and strategies to avoid them.
Find out more about the Practical Pharmacoepidemiology. Anyone with questions about the course content/suitability can contact Dr. Christopher Rentsch or Dr. Harriet Forbes at Christopher.Rentsch@lshtm.ac.uk or Harriet.Forbes@lshtm.ac.uk.
Finally, if you have any colleagues that you think would benefit from the course, do please let them know. And if there is an appropriate email group and/or noticeboard at your place of work, it would be greatly appreciated if you could circulate/post the course details to help us keep the course recruiting strongly.
Thanks!
The theatre performance ECZEMA! which is part of Professor Sinéad Langan’s Wellcome Trust funded public engagement project is now open for booking on Tuesday 4 and Wednesday 5 June. The performance takes place at the South London Gallery (65-67 Peckham Rd, London, SE5 8UH), starting at 7.30pm and has a running time of 35 minutes. To find out more, and to book tickets, please see the SLG website:
https://www.southlondongallery.org/events/eczema4jun/
https://www.southlondongallery.org/events/eczema5jun/
The performance, originally commissioned by National Theatre Wales, was updated to include outcomes from a creative writing workshop "Understanding how adult eczema affects lives" held at LSHTM in collaboration with the artist Maria Fusco in February. It is a dark comedy performed by Welsh actor Rhodri Meilir (Pride, Doctor Who) who is accompanied by organist, John Harris, who composed the score using motion-capture to translate scratching gestures (from the artist/director who has eczema herself) into music. The performance is written and directed by artist Maria Fusco and explores eczema.
The first annual lecture in memory of our greatly missed colleague Adrian Root will take place at LSHTM on Thursday 23 May. The science writer, epidemiologist and physician Ben Goldacre will be providing his unique insights into key issues around evidence-based medicine. Full details can be found on the event page.
In 2018, the EHR group launched a memorial prize, to honour the work of our colleague, Dr. Adrian Root. The prize will be awarded annually to an LSHTM MSc epidemiology student who has worked on an Electronic Health Records project. The inaugural prize was awarded to Ms. Amanda Clery at the LSHTM graduation ceremonies on March 5 2019. Amanda completed a cohort study investigating the effects of quality of antenatal care on the risk of stillbirth in the UK using the data from the Clinical Practice Research Datalink. She was supported by EHR group members Rohini Mathur (project supervisor), Caroline Minassian, and Liam Smeeth.
“We wanted to connect with people”.
As researchers we work with data; millions of lines of code, statistics and figures, tables and graphs, funnel plots indicating patterns and outliers. But we always need to remind ourselves that every line of data, every entry in a medical record or hospital database, relates to an individual journey. We got involved with cancer research for different reasons but ultimately we are all passionate about improving outcomes for cancer patients, the individuals behind the data that we use to investigate and understand the disease.
Unlike biomedical research into cancer, involving drugs or treatments, clinical trials or patient level studies, there is less of an obvious way for epidemiologists and statisticians to engage with the public and involve patients in our research. What we do is often not well understood and the value of health data for research is sometimes overlooked.
For all these reasons, we wanted to step away from our computer screens and the data, and connect with those affected. We wanted to interact with cancer patients and carers, to understand their experiences with the disease, and have the opportunity to share with them what we do, and how it involves them and their data, and why this is important. We wanted to open a dialogue and encourage mutual understanding, and we wanted to do this by creating a safe and open space for sharing, for reflecting and for expressing what can sometimes feel ‘inexpressible’.
What better way to do this, to bring people, strangers, together than through art? Anthony, a Research Fellow in the Electronic Health Records group at the London School of Hygiene & Tropical Medicine came up with the idea after discussing the effectiveness of art as therapy with Jayne Dent, an artist currently based in his hometown of Newcastle. She works with many artistic forms but was interested in the use of mono-printing as a form of expression. Mono-printing is a simple technique that creates a one-off ‘mono’ print on paper. It is an artistic form that does not need prior experience of art, specialist equipment or careful planning. It is an instant form of expression where images and text can be combined to produce a unique piece of work.
Anthony brought in Camille and Yuki, two other staff from the Department of Non-Communicable Disease Epidemiology, and together we put in a proposal which was awarded funding from the School’s public engagement small grants scheme. This enabled us to go ahead and prepare a workshop, facilitated by Jayne, and an exhibition in Newcastle.
With the help of the Cancer Research UK Centre in Newcastle and Maggie’s Centre at the Freeman Hospital in Newcastle, we were able to reach individuals in the local area that responded to flyers and social media postings advertising the event. The one-day workshop took place in late November 2018.
The 8 participants, including 7 cancer patients and 1 carer, that came along to the workshop were a special group of people who, through their courage and openness, and their willingness to fully engage with the experience, made the event a unique experience for everyone involved. We were delighted with the wonderful, expressive and moving prints they produced, as well as their observations of the day:
Being in the space, meeting other participants, being able to talk (and cry) freely, and being pushed to express feelings visually – all of this had a profound effect on me.
Coming together with strangers to share and learn something new was surprisingly calming …. a great way to cope with life’s traumas!
For us, the experience brought the human element to our daily work, the connection we were looking for. It provided the contact and the opportunity to talk to the participants about their individual journeys. It was a unique and valuable insight into the living with the disease.
Throughout the day we were able to tell them about the work that we do, how it relates to them and how their willingness to share their experiences, and their data, makes the research that we do both possible and relevant. It also gave us a fresh perspective on research questions and proposals we are considering, by reflecting and discussing the patients’ journey and their interactions with the healthcare system.
We also learned about the power of creative expression and the ability of art to act as both a form of release and of bringing people together. Before the project, we did not quite realise the power that art had, but watching the participants grow throughout the day, finding new ways of expressing their feelings, was extremely eye opening and gratifying. It changed us all in ways we might not have expected, and was a day we will never forget.
Anthony Matthews, Camille Maringe and Yuki Alencar
Exhibition: Our Cancer Journey – artistic expressions of living with cancer
28th March – 3rd April 2019
Newcastle City Library
Charles Avison Building
33 New Bridge Street West
Newcastle upon Tyne
NE1 8AX
Herpes zoster, caused by reactivation of the chickenpox virus, is linked to an increased risk of stroke, according to a recent systematic review by Harriet Forbes and colleagues. In the review, the risk of stroke approximately doubled in the week after herpes zoster and gradually returned to baseline over the next six months. While recent infection with, or reactivation of, other members of the herpesvirus family such as cytomegalovirus and herpes simplex virus may increase stroke risk, further high quality evidence is needed to confirm these findings. The paper, which included 41 studies, has recently been published in PLoS ONE.
The findings are explained in the following infographic:
Two systematic reviews assessing long-term outcomes in survivors of breast cancer have recently been published by members of the EHR research group.
Anthony Matthews and colleagues collated substantial randomised controlled trial and observational evidence on the effect of endocrine therapies on several specific cardiovascular diseases. 26 studies were identified, with results for seven specific cardiovascular disease outcomes. Results suggested an increased risk of venous thromboembolism in tamoxifen users compared with both non-users and aromatase inhibitor users. Results were also consistent with a higher risk of the vascular diseases myocardial infarction and angina in aromatase inhibitor users compared with tamoxifen users, but there was also a suggestion that this may be partly driven by a protective effect of tamoxifen on these outcomes. Data were limited, and evidence was generally inconsistent for all other cardiovascular disease outcomes. This review shows that although the choice of aromatase inhibitor or tamoxifen will primarily be based on the effectiveness against the recurrence of breast cancer, the individual patient’s risk of venous or arterial vascular disease should be an important secondary consideration. The full article was published in the BMJ.
Helena Carreira and colleagues looked at adverse mental health outcomes in women with a history of breast cancer. The authors reviewed 60 studies that compared adverse mental health outcomes in women with a history of breast and in women who never had cancer. The results showed compelling evidence of an increased risk of anxiety, depression and suicide, and neurocognitive and sexual dysfunctions in breast cancer survivors compared with women with no prior cancer. Evidence for other outcomes is scarcer, but breast cancer survivors have also been reported at increased risk of sleep disturbance and stress-related disorders including post-traumatic stress disorder. This review also highlighted that further population-based and longitudinal research would help to better characterize these associations, as approximately one-half of the studies were at high risk of selection bias and confounding by socio-economic status. The full article was published in the Journal of the National Cancer Institute.
ACE Inhibitors and ARBs are drugs that have transformed clinical care. There is strong randomised trial evidence for improved clinical outcomes from these drugs for patients with heart failure with reduced left ventricular function, and for proteinuric kidney disease. They are also recommended for use for the treatment of hypertension and after ischaemic heart disease. These multiple indications have led to them being one of the most commonly prescribed drug groups. However, in recent years there has been growing concern about their potential for ‘nephrotoxicity’. They are widely believed to be associated with AKI, particularly in patients who are hypovolaemic or septic.
Multiple guidelines recommend dose reduction or cessation of these drugs for patients who have developed or are at risk of AKI. However, it is often unclear whether, and when, the drugs should be restarted, particularly when patients are at risk of further AKI. We do know that patients are at high risk of readmission with cardiac failure after AKI but it is not clear how much this is due to cessation of ACEI/ARB drugs as part of AKI management. In addition, AKI itself is associated with increased risk of future adverse outcomes including mortality and development of chronic kidney disease. Do these drugs offer specific benefits after AKI? These issues are at the heart of daily clinical work, and yet there is minimal evidence to help us make these important decisions. In this nephrology journal club blog, Laurie Tomlinson discusses whether a recently published observational study on this topic provides evidence that can be applied to routine practice.
Body Mass Index (BMI), a measure of body fat, is linked to risk of death from every major cause except transport accidents, according to new research by the LSHTM Electronic Health Records Research Group.
The study is one of the largest of its kind to look at how BMI is associated with the risk of death both overall, and from a full spectrum of different causes – 3.6 million people and 367,512 deaths were included in the analysis. Overall, both low and high BMI were associated with an increased risk of death. BMI of between 21-25kg/m2 was associated with the lowest risk of dying from cancer and heart disease.
The research team used anonymised data from the UK Clinical Practice Research Datalink (CPRD) which includes data on BMI from general practitioners’ primary care records covering about 9% of the UK population. This is linked to data from the Office of National Statistics mortality database, which includes information on causes of death as recorded on death certificates. Risks of death from each major cause was calculated according to BMI, adjusting for other important factors such as age, sex, smoking status, alcohol use, and socioeconomic status.
Lead author Krishnan Bhaskaran said: “BMI is a key indicator of health. We know that BMI is linked to the risk of dying overall, but surprisingly little research has been conducted on the links to deaths from specific causes. We have filled this knowledge gap to help researchers, patients and doctors better understand how underweight and excess weight might be associated with diseases such as cancer, respiratory disease and liver disease.
“We found important associations between BMI and most causes of death examined, highlighting that body weight relative to height is linked to risk of a very wide range of conditions. Our work underlines that maintaining a BMI in the range 21-25kg/m2 is linked to the lowest risk of dying from most diseases.”
The authors acknowledge limitations of the study including that there was no information was available on the diet or physical activity levels of people included in the study so it was not possible to look at the interplay between BMI and these related factors. The full article was published in The Lancet Diabetes & Endocrinology.
Dr Charlotte Warren-Gash from the Electronic Heatlh Records Research group at LSHTM recently contributed to an episode of the BMJ Heart podcast, speaking with Dr James Rudd about the links between respiratory infections and subsequent heart attacks and strokes. Listen to the podcast.
Adults with eczema could face an increased risk of experiencing non-fatal cardiovascular disease, according to a recent study carried out by members of the Electronic Health Records Research Group at LSHTM.
The observational study involving almost 2 million people found that patients with eczema were 10-20% more likely to experience non-fatal cardiovascular disease than people without eczema, and that the risk increased with more severe disease. Using UK electronic health records from the Clinical Practice Research Datalink, Hospital Episode Statistics and data from the Office for National Statistics between 1998–2015, patients diagnosed with eczema were matched to those without on age, gender, general practice and calendar time. After adjusting for confounders such as socioeconomic status and age, the differences in cardiovascular disease risk between the two groups was analysed. Risk in severe eczema persisted even after adjusting for traditional cardiovascular risk factors that might mediate this association, including smoking and body mass index.
Patients with severe eczema were found to experience a 20% increased risk of stroke, 70% increased risk of heart failure, and 40–50% increased risk of the remaining cardiovascular outcomes, including unstable angina, myocardial infarction, atrial fibrillation and cardiovascular death. Eczema can vary over time and patients whose eczema was active for most of their follow up were also at greater risk of cardiovascular outcomes. The risk was mainly confined to patients with severe eczema, including people on oral immunosuppressive drugs, receiving phototherapy treatment for eczema or who were referred to dermatologists.
Eczema, also known as atopic eczema or atopic dermatitis, is a common systemic inflammatory condition which affects up to 10% of adults and is becoming more common globally. Symptoms include intense itch, pain and sleeplessness. It’s estimated that around 30% of eczema patients would be classified as having moderate-severe eczema.
Dr Sinead Langan said: “Eczema is a debilitating common condition. Increasing evidence suggests that severe eczema could be associated with a wider range of health problems than originally thought. Previous studies on the link between eczema and cardiovascular disease have reported mixed findings. However, these have lacked data on specific risk factors and have not assessed levels of eczema activity over time, points which our research addressed.”
The absolute risk of people with eczema experiencing a cardiovascular event is low. However, the links uncovered in this research, if robustly replicated by future studies, would support targeted screening and focus on primary prevention strategies to reduce cardiovascular disease among patients with eczema.
The full article was published in the British Medical Journal.
Some of the EHR group have just completed a London to Paris bike ride in memory of Adrian Root, a member of the group who sadly died at the end of 2017. We raised over £20,000 to set up a new prize for the MSc epidemiology in Adrian’s name. The trip included a gruelling (=hilly, & lots of angry motorists!) first 65 mile day from London to Newhaven, before a few more leisurely days through the French countryside. Arrival in Paris was made even more exciting by being just prior to the World Cup Final kick-off!
Asthma and COPD share many characteristics and symptoms, and the differential diagnosis between the two diseases can be difficult in primary care. Francis Nissen and colleagues have recently done a study to quantify how commonly patients with chronic obstructive pulmonary disease (COPD) have a concomitant diagnosis of asthma, and how commonly patients with asthma have a concomitant diagnosis of COPD in UK primary care. They found that a concurrent asthma and COPD diagnosis only affects a relative minority of patients with COPD (14.5%) or asthma (14.8%), and that asthma diagnoses may be over-recorded in people with COPD.
The study was based upon data from previous validation studies, including 400 COPD patients and 352 asthma patients from the Clinical Practice Research Datalink (CPRD), with disease status confirmed by review of questionnaires sent to general practitioners (GPs). The prevalence of concurrent asthma and of COPD in validated cases of either disease was examined based on CPRD coding, GP questionnaires and requested additional information. More than half (52.5%) of validated COPD patients had ever received a diagnostic asthma Read code. However, when considering additional evidence to support a diagnosis of asthma, concurrent asthma was only likely in 14.5% of validated COPD patients. Of the validated asthma patients, 15.1% had a diagnostic COPD Read code, although COPD was only likely in 14.8% of validated asthma patients. The full paper has just been accepted for publication in the British Journal of General Practice.
We know that some women may experience both physical and psychological changes after a diagnosis of breast cancer. In order to learn more about this, researchers in the EHR group, in collaboration with researchers at the Clinical Practice Research Datalink, are inviting women both with a previous diagnosis of breast cancer and those never diagnosed with cancer to answer some questions about their feelings and experiences. Comparing the answers from these two groups of women will help us to understand whether women who have had breast cancer are at greater risk of developing anxiety, depression or deterioration of quality of life, in the years after their cancer diagnosis. We hope that this knowledge will eventually help healthcare providers to target their resources more effectively to help prevent these problems.
Rationale
Every year, thousands of women are diagnosed with breast cancer in England. The treatments that are now available help many women to live for a long time after their cancer diagnosis.
Aim
The aim of this study is to understand if women who have had a diagnosis of breast cancer in the past have more anxiety, depression or a poorer quality of life compared to women who have not had cancer.
Study participants
We are inviting women with a history of breast cancer for 1 year or longer, and women who didn’t have cancer, to answer to short questionnaires about their quality of life and mental health. Participants in this study were randomly selected from primary care practices in England.
Results
This study is currently ongoing. The results will be made available in this page in due course.
Acknowledgments
We would like to thank all study participants for their collaboration. We would also like to thank the Independent Cancer Patients’ Voice for their help in the development of the study materials. This study is a collaboration between the London School of Hygiene & Tropical Medicine and the Clinical Practice Research Datalink (CPRD), at the Medicines and Healthcare products Regulatory Agency (MHRA).
This 30-week examined introductory course is relevant to anyone working in areas related to the risk-benefit of medicines and drug safety. Organised by members of the EHR research group and including lectures and workshops led by experts from academia, regulatory authorities and the pharmaceutical industry, the course can be followed face-to-face at LSHTM in London (3 blocks of teaching in November, February and April) or alternatively as distance learning. Find out more about the Professional Certificate in Pharmacoepidemiology & Pharmacovigilance.
Members of our group have recently published a paper investigating adverse effects of trimethoprim for the treatment of urinary tract infection.
We show that compared to other antibiotics used for the same reason, trimethoprim is associated with an increased risk of acute kidney injury (a sudden reduction in kidney function) and high potassium levels but not an increased risk of death. Both of these adverse effects (acute kidney injury and high potassium) are known side-effects of trimethoprim but previous studies have only investigated the risks in people taking drugs that are already associated with an increased risk – for example, those that block the renin-angiotensin system, such as ACE Inhibitors. We examined the risk of these problems in the general population over 65 years of age and showed that the risk was increased for everyone. However, because these outcomes are rare for most people, the absolute risk of using trimethoprim is very low for most people. The paper attracted quite a lot of interest, particularly by people jumping to point out that the effect of trimethoprim on kidney blood tests might lead to a false diagnosis of acute kidney injury – something we explored in depth in the Discussion section of the paper. Laurie Tomlinson (the senior author of the paper) also wrote a linked blog post discussing the importance of electronic health records and how the evidence they generate can be used by researchers to make prescribing safer.
Postscript
One of the key authors of this paper was our wonderful colleague Dr Adrian Root who sadly died earlier this year. We miss him very much. We are planning to create an Electronic Health Records prize in his honour, and members of our group will be cycling to Paris later in the year to raise money for this – more details to follow!
Three new three year UKRI Innovation Fund Fellowships have been awarded to researchers at LSHTM, aligned with Health Data Research UK, all three have strong links to the Electronic Health Records research group. Rosalind Eggo will be using linked health and environmental data to assess joint effects of air pollution and circulating infections on health outcomes. Caroline Minassian has developed a new algorithm to identify pregnancies in UK electronic health records in collaboration with the Clinical Practice Research Datalink, and will be using these data to study the neglected area of thyroid disease in pregnancy. Harriet Forbes will be assessing the effectiveness and cost-effectiveness of herpes zoster vaccines using data from both the UK and the USA.
We are delighted to report that LSHTM was part of a successful pan-London bid to be a founding substantive partner in Health Data Research UK, a major new initiative to further data science in the UK. The London partners are LSHTM, UCL, QMUL, Kings and Imperial. This is an exciting opportunity for LSHTM to help build a partnership across London. Computerised health related data offers enormous potential for research and health improvement. HDR UK will further the work of LSHTM in helping bring together the School’s world leading expertise in research methods with our NHS partners. We will also build on our established teaching excellence to help develop a new generation of data scientists.
Training in pharmacoepidemiology and pharmacovigilance
Develop your skills in pharmacoepidemiology, pharmacovigilance, and real-world evidence with our intensive online short courses. Learn key concepts in epidemiology, statistics, and health economics from experts in a range of sectors, including academia, regulatory, and industry.
| Block | Course title |
|---|---|
| Block 1 (November) | Introduction to Pharmacoepidemiology |
| Block 2 (February) | Introduction to Pharmacovigilance |
| Block 3 (March) | Intermediate Pharmacoepidemiology and Pharmacovigilance |
| Block 4 (October) | Real-World Evidence in Pharmacoepidemiology |
Study any Block in any order, or complete Blocks 1, 2, and 3 with a Project and Exam (in May) to achieve the Professional Certificate (30 credits).
Already know the basics? Our Real-World Evidence in Pharmacoepidemiology short course (Block 4) provides hands-on experience analysing and overcoming common sources of error when using real-world data.
Training in systematic reviews and meta-analysis
Develop your skills in systematic reviews and meta-analysis of health research with this intensive online short course. This four-day course will provide participants with a basis in the design, analysis and interpretation of quantitative systematic reviews of health research. Participants will be given grounding in all aspects involved in conducting a systematic review and meta-analysis, and will have the opportunity to gain practical experience of the tasks involved. By the end of the course participants will be equipped with the necessary skills to conduct their own high quality systematic reviews.
Other updates
Please check back soon or follow us on Twitter (@ehr_lshtm) for up-to-date information on other training and funding opportunities.